22 March 2024: Clinical Research
A Retrospective Study to Compare the Glasgow Coma Score, Pediatric Trauma Score, and Injury Severity Score and Outcomes in 118 Pediatric Trauma Patients at a Single Emergency Center in Turkey
Habibe Selmin ÖzensoyDOI: 10.12659/MSM.943501
Med Sci Monit 2024; 30:e943501
Abstract
BACKGROUND: The main causes of accidental trauma in children include road traffic accidents (RTAs) and falling from height (FFH). Rapid and accurate assessment of severity of injury is required to guide effective management. This retrospective study aimed to compare the Glasgow Coma Score (GCS), Pediatric Trauma Score (PTS), and Injury Severity Score (ISS) and outcomes for 118 pediatric trauma patients at a single Emergency Department (ED) in Turkey.
MATERIAL AND METHODS: Patients admitted to Ankara City Hospital due to high-energy trauma between November 1, 2019 and April 30, 2020 were analyzed retrospectively. Data for 118 patients with trauma by major mechanisms, aged 0-17, were collected. Demographic characteristics, trauma-related characteristics, outcomes, and GCS, PTS, and ISS values were compared. It was examined whether there was a relationship between trauma severity and prognosis. In this context, trauma severity was defined by these scores.
RESULTS: Of the 118 admitted patients, 66 (55.9%) were discharged from the ED, 33 (28%) were transferred to the intensive care unit (ICU), and 19 (16.1%) were admitted to non-ICU departments in the hospital. With hospitalization, patients with thoracic trauma (P<0.001; OR 11.1; 95% CI 3.0-40) and patients with abdominal trauma (P=0.003; OR 4.0; 95% CI 1.5-10.8) were discharged significantly less frequently than patients with other types of trauma. Patients with low ISS (P<0.001) and high PTS (P<0.001) were discharged more often. The relationship between diagnosis and hospitalization was significant (P<0.001).
CONCLUSIONS: RTA and FFH are the leading trauma mechanisms in children. Boys experience more trauma. ISS and PTS provide accurate predictions of severe and poor prognosis in pediatric trauma cases.
Keywords: Emergency Medicine, Injury Severity Score, Pediatric Emergency Medicine, Risk Factors, Trauma Centers
Introduction
According to 2022 data, 26.5% of Turkey’s population falls within the pediatric age group (0–18 years) [1]. Trauma confers high mortality and morbidity in children and is the second-most common reason for admission to the emergency department (ED), after infections [2]. In a study conducted in Turkey, the percentage of patients under the age of 18 who were seen in the ED was found to be 28.4% [3]. Another study revealed that 1 in every 4 children will experience an unintentional trauma requiring medical care every year [4]. According to United States of America (USA) data, 8.6 to 12 million children with trauma are treated in EDs every year, and this represents approximately 8.5% of the total 138 million ED visits [5]. Studies confirm that the leading cause of pediatric death in the USA is injuries and trauma [6]. In many cases, critical pediatric patients die within the first 24 hours after admission to the hospital [7]. This serious problem can be alleviated with quick triage [7]. A trained trauma team can reduce mortality by 25–30% when the patient arrives at the ED [8]. Although the mechanisms and types of accidents change as the anatomical structures, environments, and interests of children change in proportion to their ages, the most common causes of trauma in children are falls, in-vehicle and out-of-vehicle road traffic accidents (RTAs), bicycle accidents, drowning in water, burns, and child abuse [9].
The same trauma mechanisms injure more anatomical/physiological systems in children than in adults [8,10]. Multisystem injury occurs more frequently [10,11]. The anatomical structure of children also creates problems in terms of abdominal and pelvic injuries. Flexible ribs protect abdominal solid organs less well than the mature ribs of adults [8]. In addition, the bladder is less protected by the pelvis and genitourinary injuries may occur more frequently [8]. The care of trauma patients in the pediatric group has unique characteristics, and becomes an even more troublesome topic during times of disaster due to problems such as abuse and neglect [12]. Since fluid loss is also greater in children, follow-up and treatment also pose some difficulties [8,11]. Post-traumatic follow-up in children presents extra difficulties. For example, inaccurate values may be obtained during follow-up with pulse oximetry. Although a child under oxygen support is under respiratory distress, pulse oximetry values may be falsely high [11]. In a case of trauma with bleeding, hemoglobin values may be low and the amount of oxygen carried to the tissues may be insufficient. In this case, the pulse oximetry values monitored are again misleading [11].
There are multiple scoring systems commonly used in the triage of child trauma patients. One of these is the Pediatric Trauma Score (PTS), which is used to decide on the referral of patients to the trauma center [13]. Introduced in 1987, PTS was first compared with Injury Severity Score (ISS) and reported as a reliable indicator of injury severity [14]. PTS is a 6-parameter scoring system consisting of weight, airway, systolic blood pressure, central nervous system, open wounds, and skeletal system. The total score ranges from −6 to +12. A score of <8 indicates potentially significant trauma [13]. In one study, the specificity of the PTS was found to be 88.5–95% [15]. ISS provides the opportunity to anatomically measure the injury and make an objective evaluation. It gives insight into single or multiple trauma zones. It also has features that can predict mortality based on patient age and blunt injuries [16]. Recent studies suggest that ISS gives high results in children, and have therefore concluded that ISS does not work well, and alternative scoring should be used for children [17]. The Glasgow Coma Scale (GCS) was designed in 1974 to evaluate cases of traumatic brain injury and classify their severity. It was the first objective scoring system that addressed levels of consciousness [18]. In 1980, the use of GCS was recommended for evaluation of all trauma patients as part of the Advanced Trauma and Life Support recommendations [19]. In 1988, it began to be used by the World Federation of Neurosurgical Societies in the evaluation of subarachnoid hemorrhage [19]. In the following years, GCS has been included as a recommendation in many guidelines for the evaluation of trauma and critical patients [19]. GCS is still very useful in classifying the severity of pediatric traumatic brain injury [20]. Over time, subjective differences and inconsistencies regarding its use in pediatric patients have also been identified, and cautionary articles have been published in the literature on this point [21].
The aim of the present study was to analyze examinations and treatments in pediatric major trauma patients. The goal was to determine whether patients need to be evaluated in a high-capacity Turkish trauma center by looking at their PTS, ISS, and GCS scores. This center accepts and treats pediatric trauma cases in the adult ED. At the same time, it is a hospital with a very high capacity and abundant facilities, to which cases are transferred from many nearby hospitals by ground and air ambulances [22]. In this center and in this study, we aimed to obtain guiding data for emergency medicine and pediatric clinicians all over the world by examining both demographic characteristics and trauma scores for the care of pediatric traumas, which become more important in special periods of time. Therefore, this retrospective study aimed to compare GCS, PTS, and ISS scores and outcomes in 118 pediatric trauma patients at a single pediatric emergency center in Turkey.
Material and Methods
ETHICAL APPROVAL AND STUDY DESIGN:
Ethical approval of the study was received from Ankara Bilkent City Hospital Ethics Committee-2 on June 21, 2023, with number E2-23-4347. Parents or legal guardians of the patients were informed about this retrospective data analysis and informed consent was obtained. Access to the dataset was designed retrospectively. Patient data were obtained from patient hospital records. The patients in the study were cared for within the adult ED department and by the adult ED staff, due to the policies of the hospital. This hospital includes a wide array of emergency and surgical intervention and consultation facilities and pediatric intensive care units. Emergency medical interventions and surgical procedures can be performed, consultations can be made to all specialties, and there are also pediatric intensive care units in the hospital.
DATA COLLECTION:
Hospital records in the half-year period between November 1, 2019 and April 30, 2020, for 1480 trauma patients under the age of 18 (range: 0–17), were initially screened. Minor injuries were eliminated, leaving 118 pediatric trauma cases caused by high-energy mechanisms, which were included in the study. Cases involving a core injury to the abdomen, cases involving patients who were endotracheally intubated before admission to the hospital or who lost consciousness for another reason, cases with loss of data, and cases of patients who came to the ED 24 hours or more after the trauma were excluded.
TRAUMA MECHANISMS:
Within the scope of the definition of high-energy trauma taken into account during inclusion, cases due to RTAs, FFHs, and other trauma mechanisms (eg, sports-related injuries, assault, or falling from one’s own height) were evaluated. RTAs included traffic accidents involving passengers or pedestrians, motorcycle accidents, and bicycle accidents.
CALCULATING THE SCORES:
In the hospital where the study was conducted, the GCS score for all patients is routinely calculated and recorded on the first page of the patient file, so the calculated GCS scores were available in the hospital records for all included cases. To calculate the PTS and ISS scores analyzed in the study, the open-access and evidence-based software MDCalc Medical Calculator, software designed for healthcare professionals, was used. Scoring values for each patient were calculated using SPSS as were other patient data.
OUTCOME MEASURES:
Firstly, the demographic descriptive characteristics of the patients were collected, such as age and sex. Next, GCS, PTS and ISS median values were determined. The most frequently injured body region and the most common injury type were determined. The outcome and mortality of the children after visiting the ED were determined. Comparisons were made between these outcome data and GCS, PTS, and ISS scores. Another outcome measure was the trauma mechanism. The relationships between different trauma mechanisms and clinical outcomes were evaluated.
STATISTICAL ANALYSIS:
SPSS (Statistical Package for the Social Sciences, IBM Corp., Armonk, NY, USA) version 25 was used for statistical analysis. Before starting the analysis, we considered the data structure and checked whether key assumptions were met. Normality for continuous variables was checked with the “Kolmogorov Smirnov Test” and homogeneity of variance was checked with the “Levene Test Statistics”. In the analysis of categorical variables, the analyses to be performed were chosen according to the type of variable and, if necessary, the correlation coefficient. The Chi-square test and Fisher exact test were used to analyze categorical variables. The Mann Whitney U test was used for analysis of 2 independent groups. For analysis of multiple independent groups, the Kruskal Wallis test was used and post-hoc analysis was performed with the Mann Whitney U test. The Spearman correlation test was used to analyze numerical variables. The alpha error of the study was set as 0.05. Receiver operating characteristics and area-under-the-curve (AUC) tests were also performed to analyze the relationship between numerical data and hospitalization.
Results
DEMOGRAPHIC CHARACTERISTICS OF PATIENTS:
Our study included 1480 trauma patients under the age of 18 who were seen in our clinic between September 1, 2019 and April 30, 2020. Of these patients, 118 (7.9%) had high-energy trauma. The median age of the patients was 10 years (range: 0 to 17), and 68 (57.6%) of the patients were male. The most common reason for the ED visit was RTAs, which constituted 43 (36.4%) of the cases (Table 1).
CALCULATED GCS, PTS, AND ISS:
At the time of admission to the ED, the GCS median value was 15 (range: 3 to 15); ISS median value was 2 (range: 0 to 24); and PTS median value was 11 (range: 5 to 12) (Table 2).
CLINICAL OUTCOMES:
The most common body zones injured were the extremities, with 50 (42.4%) injuries to the extremities. The most common diagnosis was soft-tissue trauma, with 50 (42.4%) cases diagnosed with soft-tissue trauma. Regarding overall outcomes, 66 (55.9%) of our patients were discharged from the ED, 33 (28%) were transferred to the Intensive Care Unit (ICU), and 19 (16.1%) were admitted to a non-ICU department in the hospital. Only 1 of our patients (0.8%) died; 117 (99.2%) of the patients survived (Table 1).
There was a correlation between hospitalization/discharge status and the body zone injured: patients with thoracic trauma were discharged less frequently than those without (P<0.001; OR 11.1; 95% CI 3.0–40). Patients with abdominal trauma were discharged less frequently than those without (P<0.003; OR 4.0; 95% CI 1.5–10.8) (Table 2).
The relationship between the number of body zones injured and hospitalization was significant. There was no significant difference in number of body zones injured between the patients transferred to non-ICU hospital departments and those transferred to the ICU. Significant differences were seen, however, on the basis of discharge from the hospital: there were fewer areas of injury in discharged patients than in patients transferred to non-ICU departments or the ICU (P=0.001; Z=−4049); (P=0.001; Z=−6234) (Table 2).
Another significant difference was found in the relationship between hospitalization and mechanism of injury (P=0.012). Patients who fell from heights (41.9%) and those injured in motorcycle accidents (50%) had a higher rate of ICU referral (Table 2).
The relationship between diagnosis and hospitalization was also significant (P<0.001). More hospitalizations were required in patients with intracranial hemorrhage and multitrauma. Discharge was more common in cases involving trauma of the extremities (P=0.026) (Table 2).
COMPARISON OF CLINICAL OUTCOMES WITH GCS, PTS, AND ISS SCORES:
The relationship between GCS and hospitalization was significant (P<0.001). In the post-hoc analysis, it was seen that the difference was seen only in the patients hospitalized in the ICU. There was no significant difference in terms of GCS between the patients who were admitted to non-ICU departments in the hospital and those who were discharged (Table 2). The GCS in patients discharged from the ED was higher than the GCS for patients transferred to a non-ICU department (P<0.001, Z−3858) and patients transferred to the ICU (P<0.001, Z−3858).
The relationship between ISS and hospitalization was significant (P≤0.001). Post-hoc analysis showed that the difference was due to discharged patients. A significantly lower ISS was seen in discharged patients compared with patients admitted to a non-ICU hospital department (P≤001, Z=−3536) and patients transferred to the ICU (P≤0.001, Z=−4904). ISS has a sensitivity of 36% and specificity of 90% for hospitalization and discharge status (AUC: 0.670; 95% CI: 0.529–0.812) (Table 2).
The relationship between PTS and hospitalization was significant (P≤0.001). Post-hoc analysis showed that the difference was due to discharged patients. There was no significant difference between transfer to a non-ICU department of the hospital vs transfer to the ICU (P=0.273). Significantly higher PTS scores were observed in discharged patients than in patients admitted to non-ICU departments in the hospital (P≤0.001, Z−3568) and patients admitted to the ICU (P≤0.001, Z=−4522) (Table 2). The sensitivity of PTS for hospitalization and discharge was 68% and the specificity was 21% (AUC: 0.366; 95% CI: 0.252–0.480).
Discussion
This study evaluated 118 severely injured pediatric patients examined in a single ED. Male sex was more common. It was observed that most of the cases were RTAs, with the patient injured as a passenger. Soft-tissue injuries were predominant over other injury types, and these patients were more frequently discharged than patients with other injuries. There were more patients discharged from the ED than admitted to the ICU and other hospital departments. Patients injured in RTAs as passengers were significantly more likely to be discharged from the ED. Admission to the ICU was more common in patients with thoracic or abdominal injuries. Similarly, intracranial hemorrhages resulted in more ICU admissions. Calculated GCS and PTS scores of the cases were found to be high, and ISS scores were low.
Akay et al, in their report examining pediatric traumas in an area with high traffic density, found male sex to be dominant [9]. This is in agreement with similar literature reports and with the present study. Prakash et al, in their studies examining traumatic injury in children under the age of 12, also reported male sex more frequently [23]. Fylli et al examined similar pediatric traumatic injury incidence in the Netherlands and found a significantly higher number of boys in every age group [24]. In a similar study, Yousefzadeh et al examined 588 children with trauma to compare their scoring systems, and determined that male sex constituted 62.1% of the cases, according to the demographic data [25]. This can be considered as significant information for families and school educators to protect boys, as they appear to be at higher risk. Prakash et al reported RTAs and, secondarily, FFH as the major mechanisms in 911 pediatric trauma patients [23]. Akay et al found that in 124 cases, traffic accidents were the most common, followed by the mechanism of FFH [9]. In Yousefzadeh et al’s report, the most prominent mechanism was RTAs, a similar finding to those of both this study and others in the literature [25]. In the present study, the same 2 mechanisms (RTAs and FFHs) stood out as the most common, in the same order. Increasing road transportation and multi-story buildings may have served to expose vulnerable individuals in the pediatric age group to injury by RTAs and FFHs. The present data, which are compatible with previously reported data in the literature, are also important for preventive practices for the pediatric age group.
According to the data in the present study, GCS and PTS scores of the cases were found to be high and ISS was low. These 3 findings are known as good prognosis indicators. Although the study selected cases with major trauma, all 3 scores indicated good prognosis. Tepas et al previously reported that ISS and PTS change in a correlated and consistent manner [14]. In this regard, our findings are consistent with theirs. In our study, ISS was able to significantly predict prognosis when evaluated together with ICU and other hospitalizations. However, in our study, specificity for ISS and sensitivity for PTS were found to be high. Brown et al reported that ISS should be over 25 for major trauma [26]. In this sense, according to ISS, the traumatic injuries in our study seem not to be very severe. Delos et al also emphasized that PTS yields results that are more correlated with deaths due to injuries caused by mechanisms such as intentional trauma and firearms [27]. Looking at these reports and the scoring results in our study, we can infer that ISS and PTS give more correlated results in more severe traumatic injuries. It would be appropriate to study these 2 scores with larger patient groups and more severe trauma cases. Bal et al analyzed 106 patients evaluated in their center in Turkey and 125 cases evaluated in a pediatric trauma center in the USA. All cases in that international study, whether automobile passengers or pedestrians, were injured by the RTA mechanism. There were more pedestrian injuries in the cohort of cases in Turkey, and more passenger injuries in the US cohort. Taking into account all the data in that study, it is apparent that the mortality is higher than in our study [28]. Although this situation seems to be explained by their interest only in RTAs, other factors may also be influential. On the other hand, according to the data from both hospitals, they did not see a significant difference between GCS and ISS. However, it should be carefully considered that this comparison is only in the context of the RTA mechanism. On the other hand, both pedestrian RTAs and passenger RTAs are dangerous mechanisms. The results may be expected to be similar and not different from each other in both groups. In our study, however, statistically significant differences were revealed between mechanisms and hospitalization. ICU admission was found to be significantly higher in cases of motorcycle accidents and those injured by FFH. Considering hospitalization as the main indicator of prognosis, our study also showed significant results in terms of scoring. Current clinical experience may lead to the prediction that the mechanisms in clinical use may be signs of poor prognosis; ie, that this is already known. However, being able to deduce that the scores can be consistent and useful in terms of clinical prognosis makes the present study valuable.
The present study has some limitations. First of all, it has a retrospective design. The patients were not examined by the research clinicians and their prognoses were not followed up. Although this reduced the risk of bias, data had to be obtained only from hospital records. In addition, the study is single-centered. If it is predicted that there may be different mechanisms in different regions, better comparisons regarding trauma mechanism and other features can be made in a multicenter or even multinational study. Looking at the dataset, it is seen that there was only 1 case that resulted in death. For this reason, an analysis of the prognosis of the patients according to mortality could not be made and the scoring systems examined could not be compared with respect to mortality.
Conclusions
RTAs and FFHs are the prominent mechanisms in pediatric traumatic injuries. Boys are at greater risk of trauma. These conclusions should be taken into account for preventive health practices. Soft-tissue injuries are the most common type of injury for pediatric traumas. In cases of high-energy pediatric trauma evaluated in the ED, the predominance is those with good prognosis who are discharged home. Thoracic and abdominal injuries result in less hospitalization. Low GCS, low PTS, and high ISS were detected in the patients with poor prognosis. This leads to the conclusion that all 3 scoring methods are related to prognosis.
Tables
Table 1. Demographic characteristics, trauma mechanisms, injury patterns, and clinical outcomes of pediatric trauma patients in the emergency department.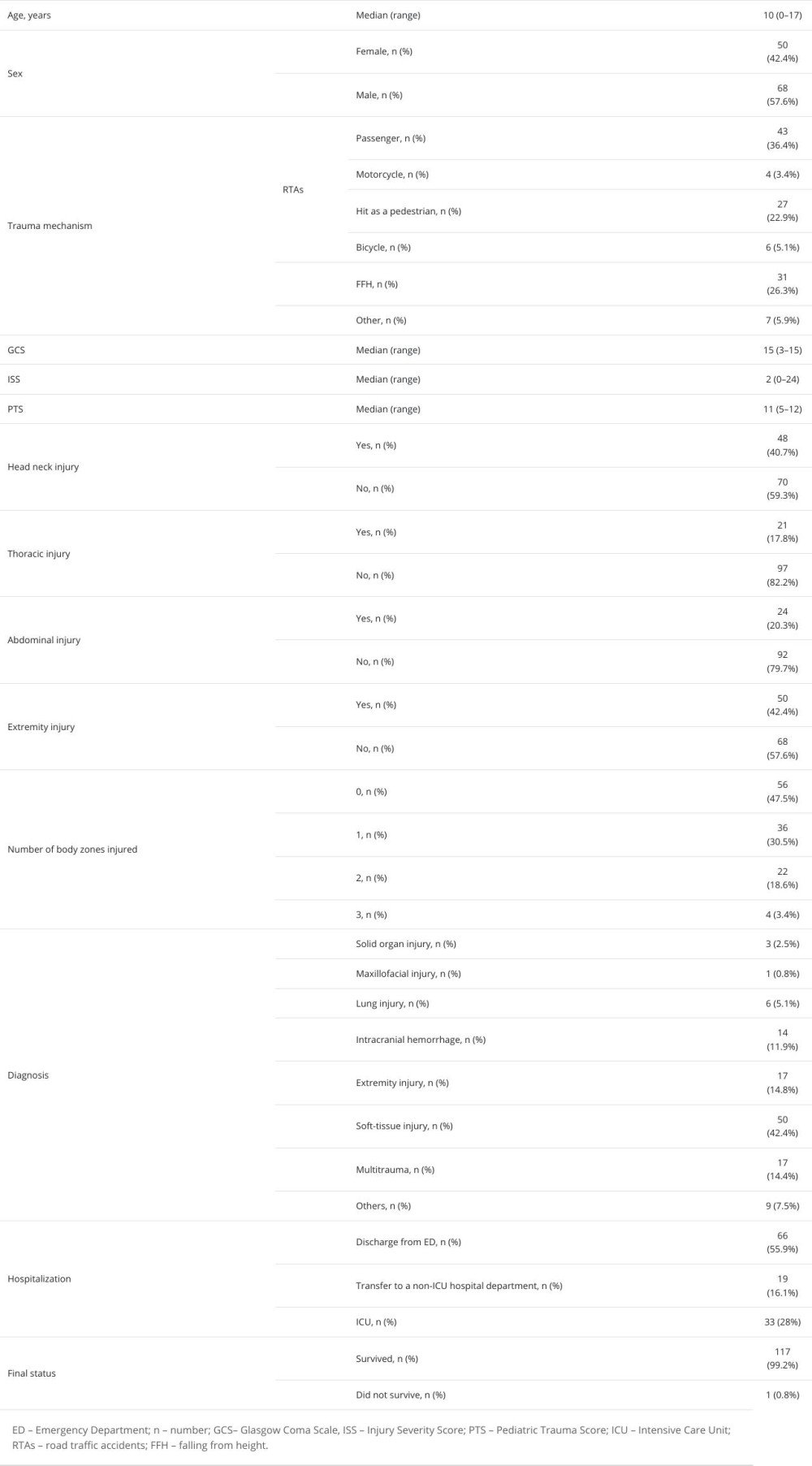 Table 2. Comparisons of age, gender, GCS, ISS, PTS, trauma mechanisms, diagnosis with outcomes of pediatric-aged trauma patients in the emergency department.
Table 2. Comparisons of age, gender, GCS, ISS, PTS, trauma mechanisms, diagnosis with outcomes of pediatric-aged trauma patients in the emergency department.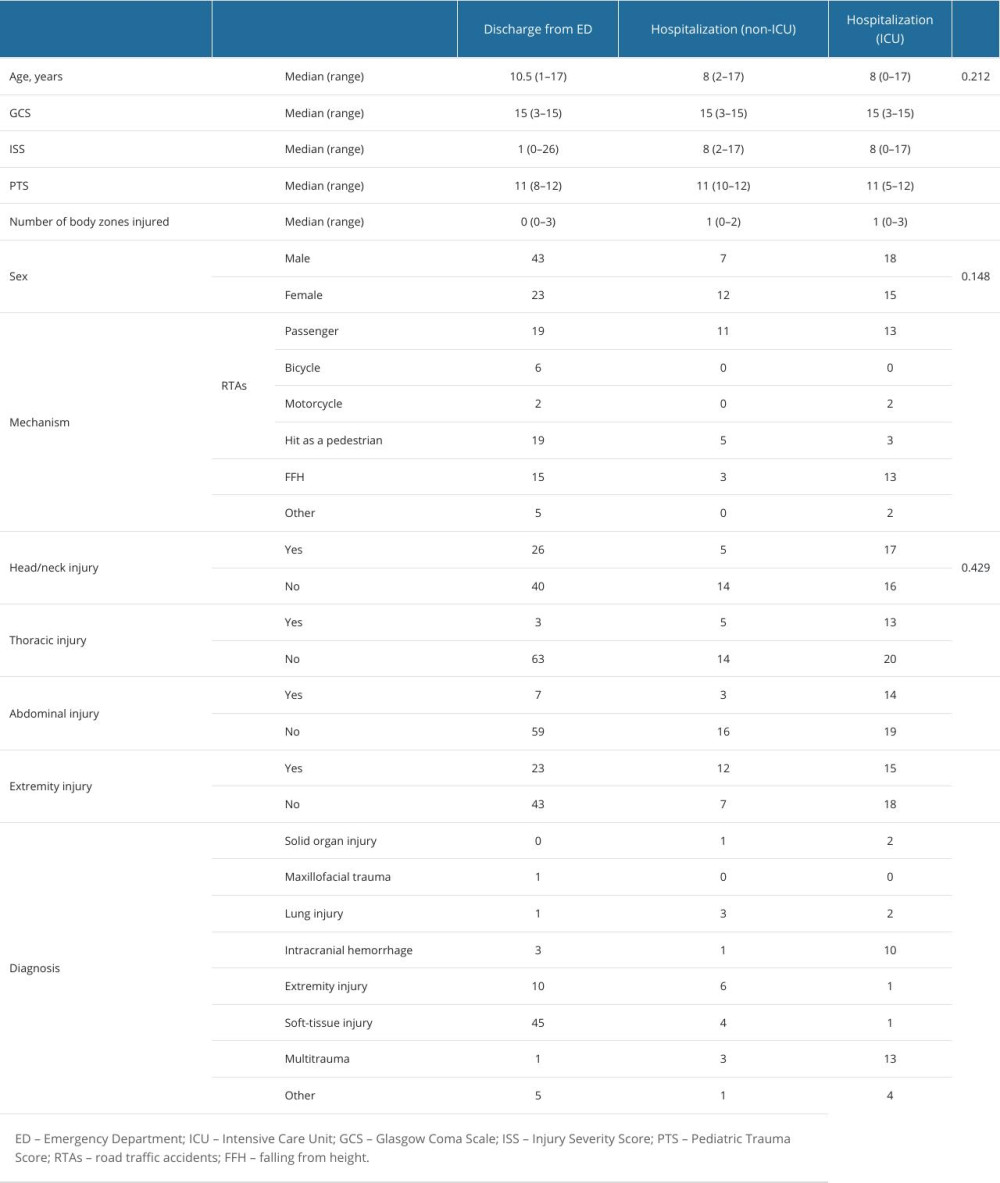
References
1. : İstatistiklerle Çocuk, 2022 Available from: [in Turkish]https://data.tuik.gov.tr/Bulten/Index?p=Istatistiklerle-Cocuk-2022-49674
2. Bambini DA, Almond PS, Abdominal trauma: Pediatric surgery, 2009; 128-83, Austin, Texas, USA, Landes Bioscience
3. Çetin Aslan E, Acil servis kullanımının değerlendirilmesi: kesitsel bir çalışma: Mersin Üniversitesi Sağlık Bilimleri Dergisi, 2023; 16(1); 1-13 [in Turkish]
4. Osterman MJ, Kochanek KD, MacDorman MF, Annual summary of vital statistics: 2012–2013: Pediatrics, 2015; 135(6); 1115-25
5. Simon TD, Bublitz C, Hambidge SJ, Emergency department visits among pediatric patients for sports-related injury: Basic epidemiology and impact of race/ethnicity and insurance status: Pediatr Emerg Care, 2006; 22(5); 309-15
6. Cunningham RM, Walton MA, Carter PM, The major causes of death in children and adolescents in the United States: N Engl J Med, 2018; 379(25); 2468-75
7. , Paediatric emergency triage, assessment and treatment: Care of critically ill children, WHO Available from: https://iris.who.int/bitstream/handle/10665/204463/9789241510219_eng.pdf;sequence=1
8. Stafford PW, Blinman TA, Nance ML, Practical points in evaluation and resuscitation of the injured child: Surg Clin North Am, 2002; 82(2); 273-301
9. Akay MA, Gürbüz N, Yayla D, Evaluation of pediatric trauma cases applied to Emergency Department: Kocaeli Med J, 2013; 2(3); 1-5
10. Avarello JT, Cantor RM, Pediatric major trauma: An approach to evaluation and management: Emerg Med Clin North Am, 2007; 25(3); 803-36
11. McFadyen JG, Ramaiah R, Bhananker SM, Initial assessment and management of pediatric trauma patients: Int J Crit Illn Inj Sci, 2012; 2(3); 121-27
12. Zaman S, Gürü S, Pediatric emergency response in a non-epicenter hospital during the 2023 Turkey-Syria earthquake: A retrospective study of 125 cases in the first 20 days: Med Sci Monit, 2023; 29; e942008
13. Lecuyer M, Calculated decisions: Pediatric Trauma Score (PTS): Pediatr Emerg Med Pract, 2019; 16(5); CD3-4
14. Tepas JJ, Mollitt DL, Talbert JL, Bryant M, The pediatric trauma score as a predictor of injury severity in the injured child: J Pediatr Surg, 1987; 22(1); 14-18
15. Jeong YS, Shah S, Akula S, Pediatric trauma smackdown: PTS vs SIPA: Injury, 2023; 54(5); 1297-301
16. Copes WS, Champion HR, Sacco WJ, The Injury Severity Score revisited: J Trauma, 1988; 28(1); 69-77
17. Hatchimonji JS, Luks VL, Swendiman RA, Settling the score: Injury Severity Score fails to capture nuances in pediatric trauma: Pediatr Emerg Care, 2022; 38(2); e828-e32
18. Teasdale G, Jennett B, Assessment of coma and impaired consciousness. A practical scale: Lancet, 1974; 2(7872); 81-84
19. Jain S, Iverson LM, Glasgow Coma Scale: StatPearls, 2023, Treasure Island (FL), StatPearls Publishing. Copyright© 2023, StatPearls Publishing LLC
20. Haydel MJ, Weisbrod LJ, Saeed W, Pediatric head trauma: StatPearls, 2023, Treasure Island (FL), StatPearls Publishing. Copyright© 2023, StatPearls Publishing LLC
21. Caruana M, Hackenbruch SN, Grech V, Farrugia R, Inconsistency in the application of Glasgow Coma Scale in pediatric patients: Med Princ Pract, 2023 [Online ahead of print]
22. Özensoy HS, Gürü S, Helicopter Ambulance transport to the Emergency Department: Demographic and clinical factors impacting outcomes in a Turkish Medical Center: Med Sci Monit, 2023; 29; e941464
23. Prakash Raju KNJ, Jagdish S, Kumar GK, Profile of pediatric trauma among the patients attending Emergency Department in a Tertiary Care Hospital in South India: J Emerg Trauma Shock, 2020; 13(1); 62-67
24. Fylli C, Schipper IB, Krijnen P, Pediatric trauma in The Netherlands: Incidence, mechanism of injury and in-hospital mortality: World J Surg, 2023; 47(5); 1116-28
25. Yousefzadeh-Chabok S, Kazemnejad-Leili E, Kouchakinejad-Eramsadati L, Comparing pediatric trauma, Glasgow Coma Scale and Injury Severity scores for mortality prediction in traumatic children: Ulus Travma Acil Cerrahi Derg, 2016; 22(4); 328-32
26. Brown JB, Gestring ML, Leeper CM, The value of the injury severity score in pediatric trauma: Time for a new definition of severe injury?: J Trauma Acute Care Surg, 2017; 82(6); 995-1001
27. De Los Ríos-Pérez A, García A, Cuello L, Performance of the Paediatric Trauma Score on survival prediction of injured children at a major trauma centre: A retrospective Colombian cohort, 2011–2019: Lancet Reg Health Am, 2022; 13; 100312
28. Bal A, Cooper M, Lee A, The evaluation of trauma care: The comparison of 2 High-Level Pediatric Emergency Departments in the United States and Turkey: Pediatr Emerg Care, 2019; 35(9); 611-17
Tables
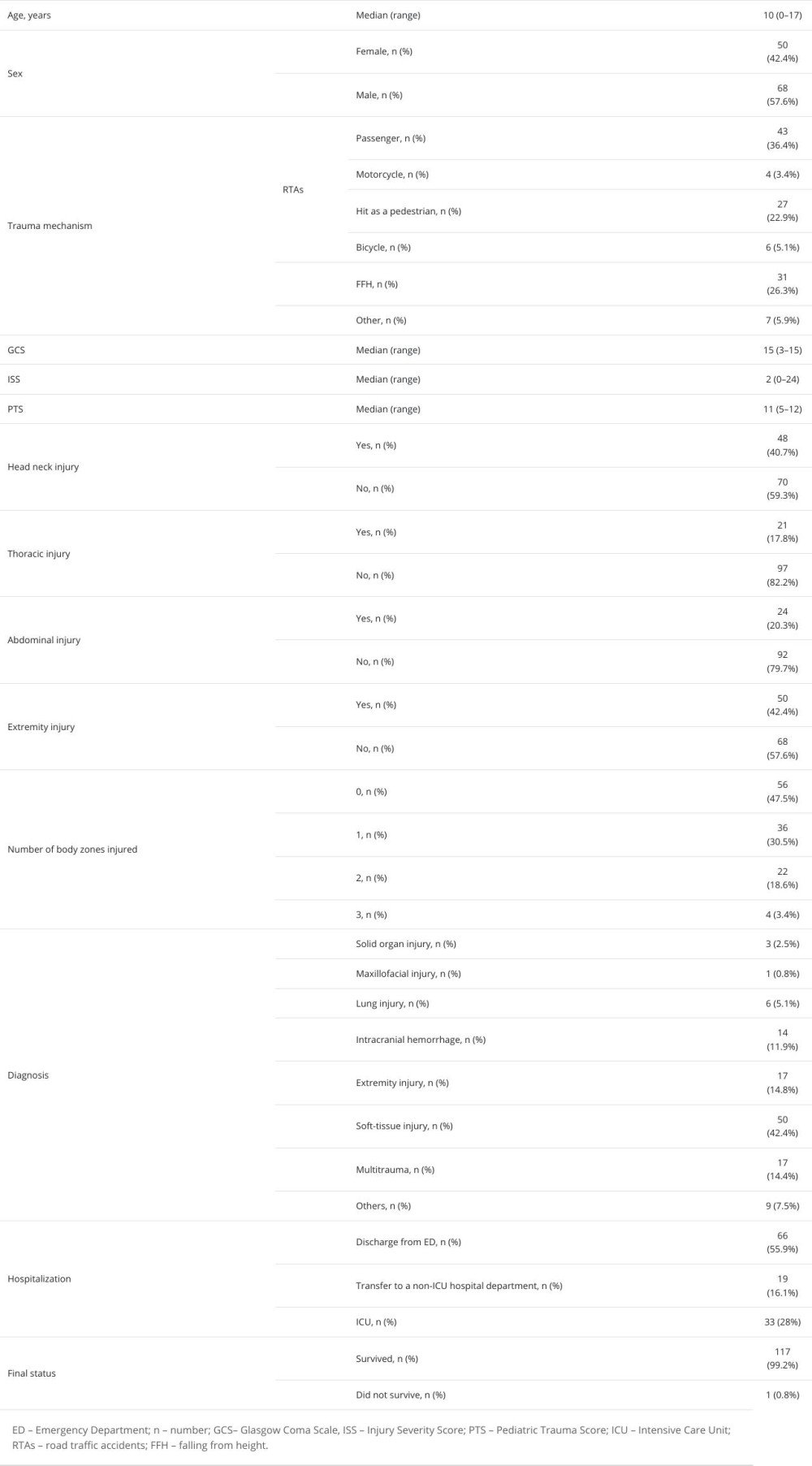 Table 1. Demographic characteristics, trauma mechanisms, injury patterns, and clinical outcomes of pediatric trauma patients in the emergency department.
Table 1. Demographic characteristics, trauma mechanisms, injury patterns, and clinical outcomes of pediatric trauma patients in the emergency department.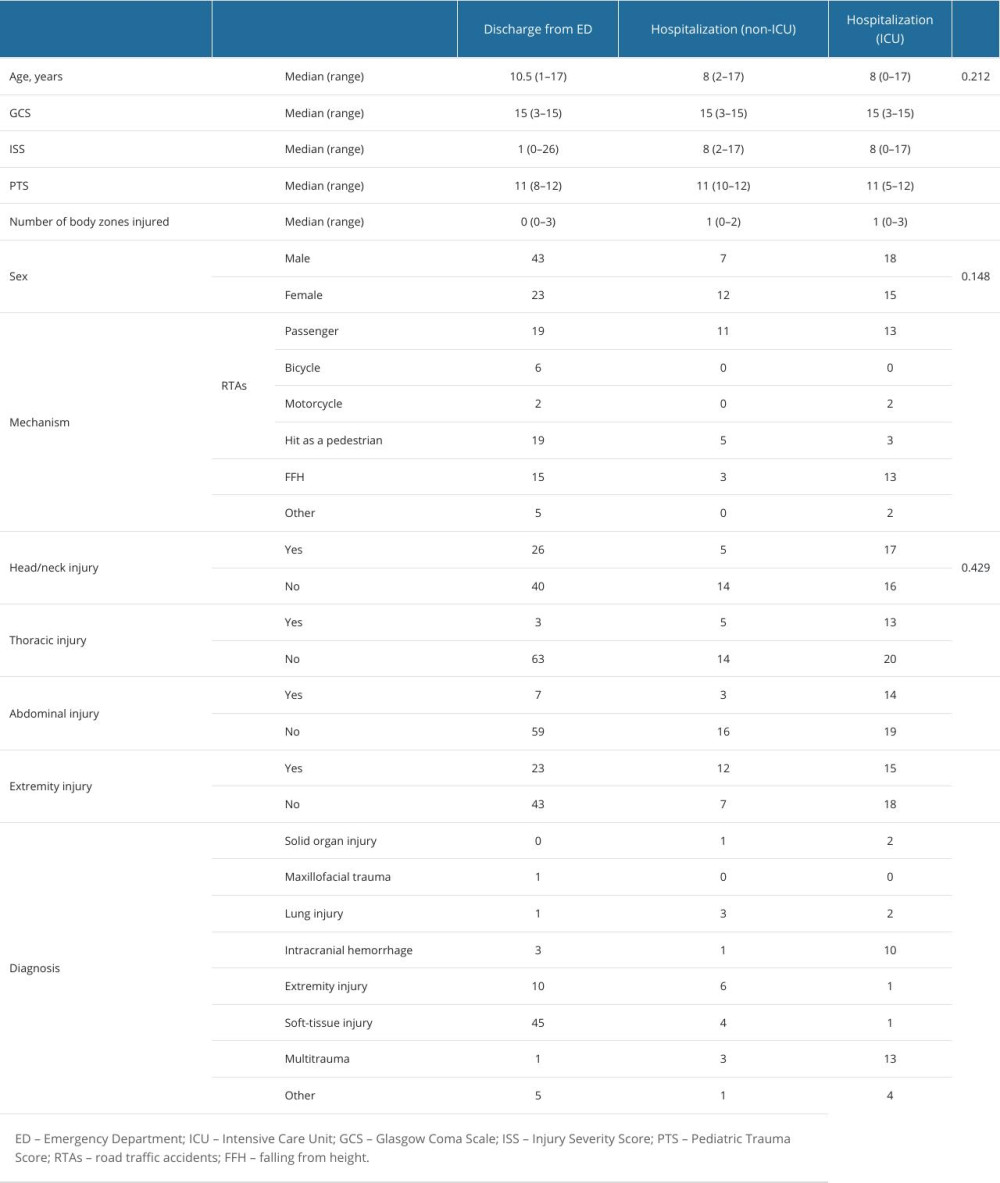 Table 2. Comparisons of age, gender, GCS, ISS, PTS, trauma mechanisms, diagnosis with outcomes of pediatric-aged trauma patients in the emergency department.
Table 2. Comparisons of age, gender, GCS, ISS, PTS, trauma mechanisms, diagnosis with outcomes of pediatric-aged trauma patients in the emergency department. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








