06 April 2024: Clinical Research
Nutritional Status and Quality of Life in Patients with Oral Squamous Cell Carcinoma Before and After Surgical Oncological Treatment: A Single-Center Retrospective Study
Miloš Z. Stojanović1ABDEF*, Dragan Krasić1ADF, Predrag Radović1B, Miloš Trajkovic1B, Andrija Ćosić1B, Vladimir Petrović2DEF, Pavle PešićDOI: 10.12659/MSM.943844
Med Sci Monit 2024; 30:e943844
Abstract
BACKGROUND: Oral squamous cell carcinoma (OSCC) is the most common of head and neck malignancies in well-developed countries. In most cases, patients with OSCC experience a degree of nutritional status disturbances and decreased quality of life (QoL). This study aimed to compare nutritional status and QoL in 51 patients before and after surgery for OSCC.
MATERIAL AND METHODS: Fifty-one eligible patients with OSCC were followed during a 3-year period (2019-2022). For all patients, we determined body mass index (BMI), serum albumin (ALB), prognostic nutritional index, and nutritional risk index before and after treatment. Also, all patients completed a standardized QoL questionnaire before and after treatment. The obtained data were compared between the groups by using the t test and multivariate Cox regression.
RESULTS: The values of BMI and NRI were statistically significantly different between the preoperative and postoperative measurements (24.1 kg/m² vs 21.1 kg/m², and 103 vs 100.1, respectively, P=0.001), while values of ALB and prognostic nutritional index did not differ significantly (41.35 g/L vs 39.1 g/L, and 48.5 vs 46.2, respectively). Dysphagia (P=0.03) and chewing problems (P=0.04) were found to be the 2 most important factors decreasing the QoL of patients.
CONCLUSIONS: Based on our results, BMI and NRI were the most sensitive parameters of nutritional status. Dysphagia and chewing problems were the 2 most important factors affecting the QoL in patients with OSCC.
Keywords: Squamous Cell Carcinoma of Head and Neck, Body Mass Index, Serum Albumin, Nutritional Status, Quality of Life
Introduction
Oral squamous cell carcinoma (OSCC) has the highest incidence of head and neck malignancies, which has been consistently increasing in prevalence, particularly in well-developed countries [1,2]. According to the available data, OSCC makes up more than 90% of oropharyngeal cancers [3]. OSCC has an unpredictable prognosis, with reported 5-year survival rates of approximately 50% [1]. There are 2 types of OSCC: the first type is caused by human papillomavirus infection, while the second is mainly due to tobacco smoking and alcohol use. The diagnosis of OSCC is made based on biopsy results of the affected tissue. Treatment involves surgery, radiotherapy, chemotherapy, or a combination of these therapies [3].
In most cases, patients with OSCC already on their first clinical presentation experience a degree of nutritional status disturbances and weight loss [4]. These are determined by the anatomical location and extent of the tumor process, with impaired functions of swallowing and chewing. Therefore, almost half of patients with OSCC have a degree of malnutrition at the time of first examination [5]. Some studies have confirmed a direct association between malnutrition and survival rates [6]. In general, the tumor process and surgical and oncological therapy, as standard treatments of OSCC, contribute to malnutrition, with body mass and albumin losses [7], which leads to nutritional status impairment, weakened immunity, and increased incidence of post-treatment complications.
Patients with OSCC, as already known, have a decreased quality of life (QoL) at the time of presentation, above all in the sense of impaired swallowing, speech, chewing, and presence of pain. Additional surgical oncological treatment leads to further aggravation of these QoL parameters.
The patients affected with oral carcinoma represent an especially vulnerable population because the presence of the tumor usually leads to difficulties in eating, both before and after surgical and oncological treatment. Consequently, the risk of malnutrition is increased, which represents an additional risk factor for the successful recovery by causing susceptibility to infections and complications during treatment [8]. The problem of malnutrition in patients with cancer is not sufficiently addressed in clinical facilities, and the metabolic changes that occur because of malnourishment are not often properly treated. The reduced food intake leads to the loss of weight and muscle mass and the activation of a catabolic metabolic state, which together increase the risk of postoperative complications and prolonged recovery time [9]. However, the patients’ personal traits, diminished QoL, psychological state, and fear for the future should also be considered, as they significantly influence the recovery process [10].
Earlier studies have confirmed that the most frequently used parameters of nutritional status assessment in cancer patients are body mass index (BMI) and serum albumin (ALB), including patients with OSCC, rectal cancer, and others [11,12]. In more recent studies, the following 2 new parameters, the prognostic nutritional index (PNI) and nutritional risk index (NRI), have been proposed [1]. The PNI combines ALB with lymphocyte counts, while the NRI combines body mass, height, and ALB.
This questionnaire-based retrospective study from a single center aimed to compare nutritional status and QoL in 51 patients before and after surgery for OSCC.
Material and Methods
INCLUSION AND EXCLUSION CRITERIA:
We examined the nutritional status and QoL of 51 eligible patients with OSCC and subsequently treated surgically and with adjuvant radiation or chemoradiation therapy, as established by the European Association for Cranio-Maxillofacial Surgery algorithm for patients with OSCC. The inclusion and exclusion criteria were in accordance with the study by Pingili et al [13]. We included patients who were older than 18 years, diagnosed with OSCC (confirmed by histopathology), and underwent surgical and oncological treatment. Exclusion criteria were patients with distant metastases and T4 stage of disease, patients with biopsy only (without surgical therapy), patients with oropharyngeal carcinoma, patients who failed to complete the treatment, and those with complex surgical reconstructions.
NUTRITIONAL STATUS AND QOL PARAMETERS:
The following patient information was collected: sex, age, height, weight, tumor anatomical site, tumor-node-metastasis (TNM) classification of the tumor, ALB, and lymphocyte count (pre- and post-treatment values). All patients were asked to complete a QoL questionnaire before and after treatment (European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, Core Module [QLQ-C30] and Head and Neck Module [QLQ-H&N35]) [10]. The mean time from surgery to treatment completion (radiation or chemoradiation) was no longer than 4 months. The serological parameters were obtained at the Center for Medical and Clinical Biochemistry of the University Clinical Center in Nis, Serbia.
Before and after treatment completion, BMI, PNI, and NRI were was calculated as follows:
STATISTICAL ANALYSIS:
The results are presented as frequencies and percentages or as means within intervals. The data were collected and presented in the form of tables (MS Office Excel, Microsoft Corp, Redmond, WA, USA). Descriptive statistical analyses were done using the software package SPSS, v. 20.0 (IBM Corp, Armonk, NY, USA).
BMI, ALB, PNI, NRI, and QLQ pre- and post-treatment values were compared using the
Results
DEMOGRAPHIC AND CLINICAL CHARACTERISTICS:
The study enrolled 51 patients over 3 years. Patient ages ranged from 23 to 85 years (average 54), with 35 men and 16 women (2.19: 1 male-to-female ratio).
The tongue was the most affected site by cancer (26 cases, 51%), followed by the mouth floor (7 cases, 15%). Both anatomical sites were simultaneously involved in 13 cases (26%). According to TNM classification, 23 patients (45%) had T2N1M0 disease, while 15 patients (30%) had T2N0M0 disease. Basic demographic and clinical patient characteristics are presented in Table 1.
NUTRITIONAL STATUS PARAMETERS:
The pretreatment mean value of BMI was 24.1 kg/m2 (16.65–31.65 kg/m2) and ALB was 41.35 g/L (30.5–46.4 g/L). The post-treatment mean value of BMI was 21.1 kg/m2 (14.30–27.48 kg/m2), and ALB was 39.1 g/L (32.2–49.3 g/L). PNI and NRI pretreatment values were 48.5 (40.5–57.5) and 103 (90.9–116), while their post-treatment values were 46.2 and 100.1, respectively.
Following the WHO definition, BMI <20, ALB <40g/L, PNI <49.3, and NRI <97.5 were used to identify patients with malnourishment. Regarding nutritional status, 13 patients (25.5%) were malnourished according to their pretreatment BMI, while 17 patients (33.3%) were normally nourished, and 21 patients (42%) had obesity. According to their post-treatment BMI, 23 patients (45%) were malnourished, 8 patients (14.5%) were normally nourished, and 10 patients (20%) had obesity.
In the studied period, the values of BMI and NRI statistically significantly changed from before to after treatment (P<0.05). The values of albumin and PNI did not change statistically significantly between the 2 measurements (Table 2).
From before to after treatment, BMI and NRI values significantly decreased in male and female patients. It was also found that albumin and PNI values did not differ significantly between the 2 measurements.
Cox multivariate regression demonstrated strong associations between PNI and ALB (r=0.77), NRI and ALB (r=0.70), NRI and BMI (r=0.73), and NRI and PMI (r=0.62). There were weak associations between ALB and BMI (r=0.15) and PNI and BMI (r=0.20) (Table 3).
QOL PARAMETERS:
The EORTC QLQ-C30 and H&N35 questionnaires were used to analyze dysphagia, pain, chewing, social activity, and psychological status. The frequency and P values of these parameters in the pretreatment and post-treatment groups are shown in Table 4.
Discussion
LIMITATIONS OF THE STUDY:
The present study had a relatively small sample size (51 patients), lasted for a relatively short time, and was conducted in a single center. In addition, we did not enroll patients in supportive nutritional therapy, which has been suggested in various studies as an effective tool for preventing and managing malnutrition [4]. We plan to do this in future studies because nutritional support, as shown previously, can improve QoL and reduce malnutrition incidence [52,53].
Conclusions
The results of our study demonstrated that the combination of BMI and NRI was the most sensitive parameter of nutritional status in postoperative patients with OSCC. Also, the most common symptoms affecting QoL were dysphagia and chewing problems, which in turn can further aggravate malnutrition in patients with OSCC. The results also showed the importance of nutrition in patients with OSCC, one of the essential factors of treatment success and complete rehabilitation of these patients.
Therefore, future studies need to focus on the standardization of analysis of nutritional status for patients with OSCC, identification of the most suitable analysis parameters, and use of a multidisciplinary approach to identify biochemical, surgical, oncological, and psychological complications that this type of cancer can cause. Also, it is important to establish the precise indications for inpatient and outpatient enteral supportive therapy to avoid possible pre- and post-treatment complications and to thoroughly analyze its importance in maintaining or improving the nutritional status of patients with OSCC.
Tables
Table 1. Basic demographic and clinical characteristics of patients.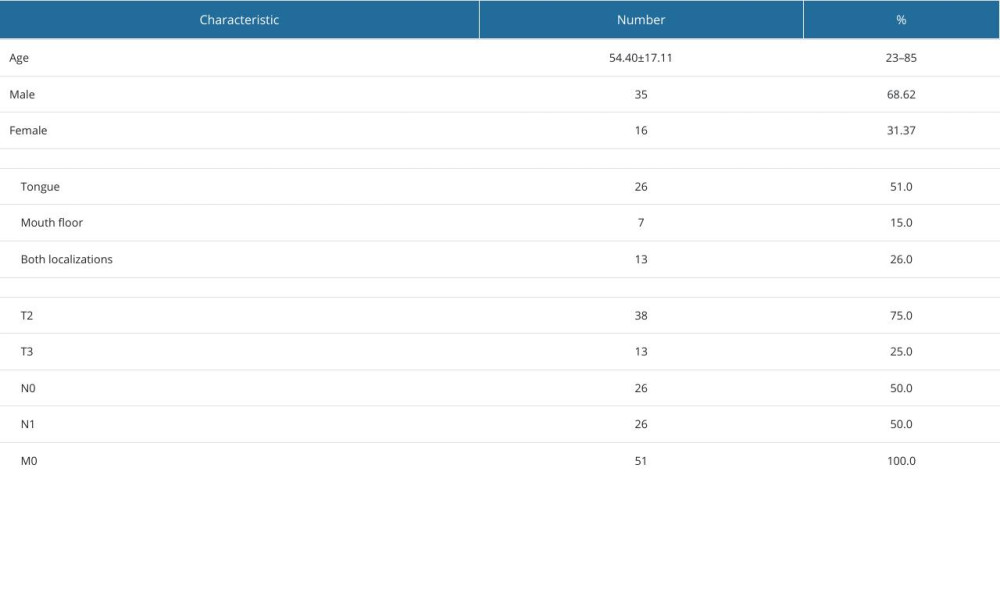 Table 2. Pre- and post-treatment body mass index (BMI), serum albumin (ALB), prognostic nutritional index (PNI), and nutritional risk index (NRI) values.
Table 2. Pre- and post-treatment body mass index (BMI), serum albumin (ALB), prognostic nutritional index (PNI), and nutritional risk index (NRI) values. Table 3. Cox multivariate regression analysis between the examined parameters.
Table 3. Cox multivariate regression analysis between the examined parameters.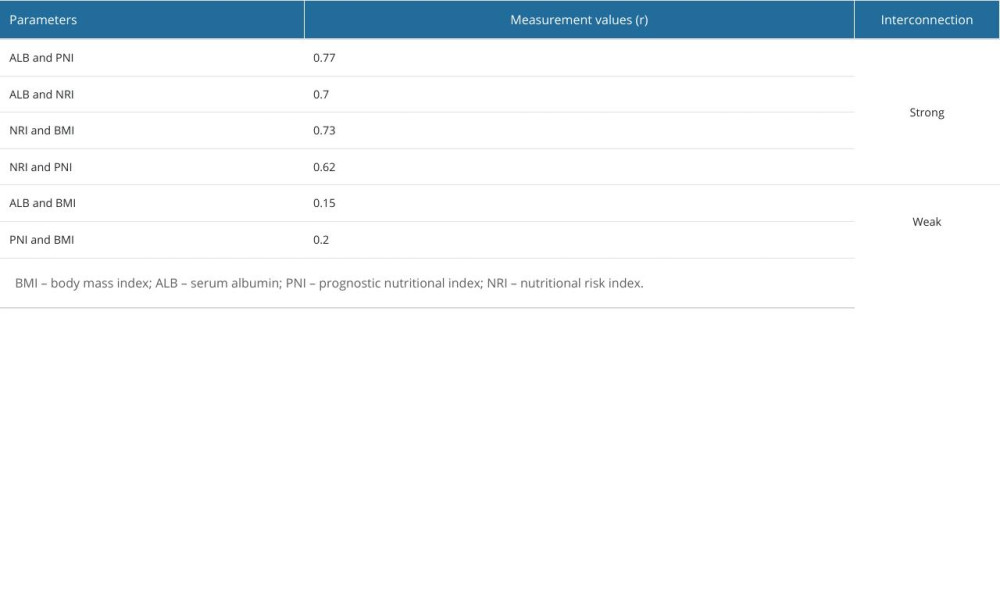 Table 4. Frequency of pretreatment and post-treatment quality of life parameters.
Table 4. Frequency of pretreatment and post-treatment quality of life parameters.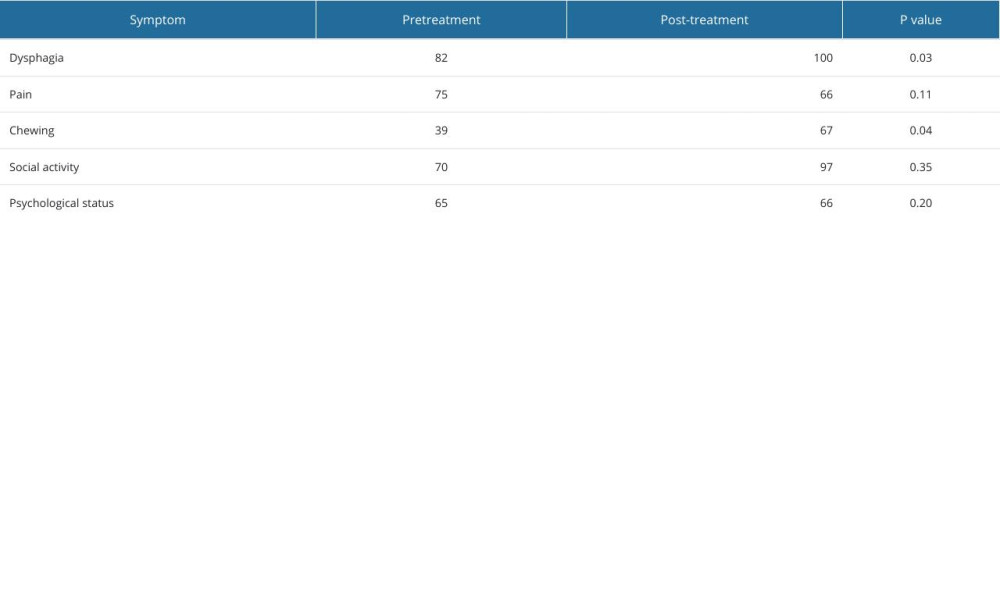
References
1. Bao X, Liu F, Lin J, Chen Q, Nutritional assessment and prognosis of oral cancer patients: A large-scale prospective study: BMC Cancer, 2020; 20(1); 146
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries: CA Cancer J Clin, 2018; 68(6); 394-424
3. Jamal Z, Anjum F, Oropharyngeal squamous cell carcinoma[Updated 2023 Apr 27]: StatPearls [Internet], 2024, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK563268/
4. Stojanović M, Krasić D, Papović M, Frequency of malnutrition in patients with intraoral carcinoma: Acta Medica Medianae, 2023; 62(4); 22-28
5. Tsai YT, Lai CH, Huang TH, Association of malnutrition with postoperative complication risk after curative surgery for oral cancer. Observational study: Medicine (Baltimore), 2020; 99(52); e23860
6. Kono T, Sakamoto K, Shinden S, Ogawa K, Pre-therapeutic nutritional assessment for predicting severe adverse events in patients with head and neck cancer treated by radiotherapy: Clin Nutr, 2017; 36(6); 1681-85
7. Yanni A, Dequanter D, Lechien JR, Malnutrition in head and neck cancer patients: Impacts and indications of a prophylactic percutaneous endoscopic gastrostomy: Eur Ann Otorhinolaryngol Head Neck Dis, 2019; 136(3S); S27-S33
8. Bao X, Liu F, Lin J, Nutritional assessment and prognosis of oral cancer patients: A large-scale prospective study: BMC Cancer, 2020; 20(1); 146
9. Nett H, Steegmann J, Tollkühn-Prott B, A prospective randomized comparative trial evaluating postoperative nutritional intervention in patients with oral cancer: Sci Rep, 2022; 12(1); 14213
10. Gellrich NC, Handschel J, Holtmann H, Krüskemper G, Oral cancer malnutrition impacts weight and quality of life: Nutrients, 2015; 7(4); 2145-60
11. Saroul N, Pastourel R, Mulliez A, Which assessment method of malnutrition in head and neck cancer?: Otolaryngol Head Neck Surg, 2018; 158(6); 1065-71
12. Liu F, Chen F, Huang J, Prospective study on factors affecting the prognosis of oral cancer in a Chinese population: Oncotarget, 2017; 8(3); 4352-59
13. Pingili S, Ahmed J, Sujir N, Evaluation of malnutrition and quality of life in patients treated for oral and oropharyngeal cancer: ScientificWorldJournal, 2021; 2021; 9936715
14. Cervino G, Fiorillo L, Herford AS, Molecular biomarkers related to Oral carcinoma: Clinical trial outcome evaluation in a literature review: Dis Markers, 2019; 2019; 8040361
15. Eskander A, Kang S, Tweel B, Predictors of complications in patients receiving head and neck free flap reconstructive procedures: Otolaryngol Head Neck Surg, 2018; 158(5); 839-47
16. Rathod S, Gupta T, Ghosh-Laskar S, Quality-of-life (QOL) outcomes in patients with head and neck squamous cell carcinoma (HNSCC) treated with intensity-modulated radiation therapy (IMRT) compared to three-dimensional conformal radiotherapy (3D-CRT): Evidence from a prospective randomized study: Oral Oncol, 2013; 49(6); 634-42
17. Kubrak C, Olson K, Jha N, Nutrition impact symptoms: key determinants of reduced dietary intake, weight loss, and reduced functional capacity of patients with head and neck cancer before treatment: Head Neck, 2010; 32(3); 290-300
18. Liu SA, Tsai WC, Wong YK, Nutritional factors and survival of patients with oral cancer: Head Neck, 2006; 28(11); 998-1007
19. Leung JS, Seto A, Li GK, Association between preoperative nutritional status and postoperative outcome in head and neck cancer patients: Nutr Cancer, 2017; 69(3); 464-69
20. Danan D, Shonka DC, Selman Y, Prognostic value of albumin in patients with head and neck cancer: Laryngoscope; 126(7); 1567-71 016
21. Shah MA, Capanu M, Soff G, Risk factors for developing a new venous thromboembolism in ambulatory patients with nonhematologic malignancies and impact on survival for gastroesophageal malignancies: J Thromb Haemostasis, 2010; 8(8); 1702-9
22. Douglas E, McMillan DC, Towards a simple objective framework for the investigation and treatment of cancer cachexia: The Glasgow prognostic score: Cancer Treat Rev, 2014; 40(6); 685-91
23. Dunn GP, Bruce AT, Ikeda H, Cancer immunoediting: From immunosurveillance to tumor escape: Nat Immunol, 2002; 3(11); 991-98
24. Shoji F, Morodomi Y, Akamine T, Predictive impact for postoperative recurrence using the preoperative prognostic nutritional index in pathological stage I non-small cell lung cancer: Lung Cancer, 2016; 98; 15-21
25. Mohri T, Mohri Y, Shigemori T, Impact of prognostic nutritional index on long-term outcomes in patients with breast cancer: World J Surg Oncol, 2016; 14(1); 170
26. Jin S, Cao S, Xu S, Clinical impact of pretreatment prognostic nutritional index (PNI) in small cell lung cancer patients treated with platinum-based chemotherapy: Clin Respir J, 2018; 12(9); 2433-40
27. Fujiya K, Kawamura T, Omae K, Impact of malnutrition after gastrectomy for gastric cancer on long-term survival: Ann Surg Oncol, 2018; 25(4); 974-83
28. Bo Y, Yao M, Zhang L, Preoperative nutritional risk index to predict postoperative survival time in primary liver cancer patients: Asia Pac J Clin Nutr, 2015; 24(4); 591-97
29. Chen F, Lin L, Liu F, Three prognostic indexes as predictors of response to adjuvant chemoradiotherapy in patients with oral squamous cell carcinoma after radical surgery: A large-scale prospective study: Head Neck, 2019; 41(2); 301-8
30. Silander E, Nyman J, Hammerlid E, An exploration of factors predicting malnutrition in patients with advanced head and neck cancer: Laryngoscope, 2013; 123(10); 2428-34
31. World Health Organization. WHO Expert Committee on Medical Rehabilitation, Second Report: World Health Organ Tech Rep Ser, 1969; 419; 1-23
32. Dzebo S, Mahmutovic J, Erkocevic H, Quality of life of patients with oral cavity cancer: Mater Sociomed, 2017; 29(1); 30-34
33. Ghorbani Z, Manifar S, Bohloli G, Oral health-related quality of life in patients with oral squamous cell carcinoma: A case-control study: Dent Res J (Isfahan), 2023; 20; 36
34. Gondivkar SM, Gadbail AR, Sarode SC, Oral and general health-related quality of life in oral squamous cell carcinoma patients – comparative analysis of different treatment regims: J Oral Biol Craniofac Res, 2021; 11(2); 125-31
35. Valdez JA, Brennan MT, Impact of oral cancer on quality of life: Dent Clin North Am, 2018; 62(1); 143-54
36. Kamstra JI, Jager-Wittenaar H, Dijkstra PU, Oral symptoms and functional outcome related to oral and oropharyngeal cancer: Support Care Cancer, 2011; 19(9); 1327-33
37. de Graeff A, de Leeuw JR, Ros WJ, Pretreatment factors predicting quality of life after treatment for head and neck cancer: Head Neck, 2000; 22(4); 398-407
38. Terrell JE, Welsh DE, Bradford CR, Pain, quality of life, and spinal accessory nerve status after neck dissection: Laryngoscope, 2000; 110(4); 620-26
39. Biazevic MG, Antunes JL, Togni J, Immediate impact of primary surgery on health-related quality of life of hospitalized patients with oral and oropharyngeal cancer: J Oral Maxillofac Surg, 2008; 66(7); 1343-50
40. Agarwal SK, Munjal M, Koul R, Agarwal R, Prospective evaluation of the quality of life of oral tongue cancer patients before and after the treatment: Ann Palliat Med, 2014; 3(4); 238-43
41. Sisolefsky F, Rana M, Rana M, Determinants of quality of life from the perspective of patients: A qualitative analysis of patients with oral cancer: J Craniomaxillofac Surg, 2021; 49(1); 59-63
42. Chan Y, Irish JC, Wood SJ, Patient education and informed contest in head and neck surgery: Arch Oto-laryngol Head Neck Surg, 2002; 128(11); 1269-74
43. Nagy J, Braunitzer G, Antal M, Quality of life in head and neck cancer patients after tumor therapy and subsequent rehabilitation: An exploratory study: Qual Life Res, 2014; 23(1); 135-43
44. Rinkel RN, Verdonck-de Leeuw IM, The psychometric and clinical validity of the SWAL-QOL questionnaire in evaluating swallowing problems experienced by patients with oral and oropharyngeal cancer: Oral Oncol, 2009; 45(8); e67-71
45. van den Berg MG, Rasmussen-Conrad EL, van Nispen L, A prospective study on malnutrition and quality of life in patients with head and neck cancer: Oral Oncol, 2008; 44(9); 830-37
46. Leung JS, Seto A, Li GK, Association between preoperative nutritional status and postoperative outcome in head and neck cancer patients: Nutr Cancer, 2017; 69(3); 464-69
47. Dort JC, Farwell DG, Findlay M, Optimal perioperative care in major head and neck cancer surgery with free flap reconstruction a concensus review and recommendations from the Enchanced Recovery After Surgery Society: JAMA Otolaryngol Head and Neck Surg, 2017; 143(3); 292-303
48. Coyle MJ, Main B, Hughes C, Enchanced recovery after surgery (ERAS) for head and neck oncology patients: Clin Otolaryngol, 2016; 41(2); 118-26
49. Aires FT, Dedivitis RA, Petrarolha SM, Early oral feeding after total laryngectomy: Sistematic review: Head Neck, 2015; 37(10); 1532-35
50. Bermazović M, Panisić M, Popadic A, Rondovic GERAS program in elective surgery: NUPENS, 2021; 113-117 Available from: [in Bosnian]www.researchgate.net/publication/357605538_PREPORUKE_Nacionalnog_Udruzenja_za_klinicku_ishranu_Srbije_u_elektivnoj_hirurgiji_ERAS_program_u_elektivnoj_hirurgiji
51. Talwar B, Findlay M, When is the optimal time for plaing a gastrostomy in patients undergoing treatment for head and neck cancer?: Curr Opin Support Palliat Care, 2012; 6(1); 41-53
52. Jain PV, Bang B, Manikantan K, Factors affecting postoperative complications after reconstructive surgery in oral carcinoma patients: A prospective study of 100 patients: Indian J Otolaryngol Head Neck Surg, 2019; 71(Suppl 1); 341-47
53. Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME, Impact of nutrition on outcome: A prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy: Head Neck, 2005; 27(8); 659-68
Tables
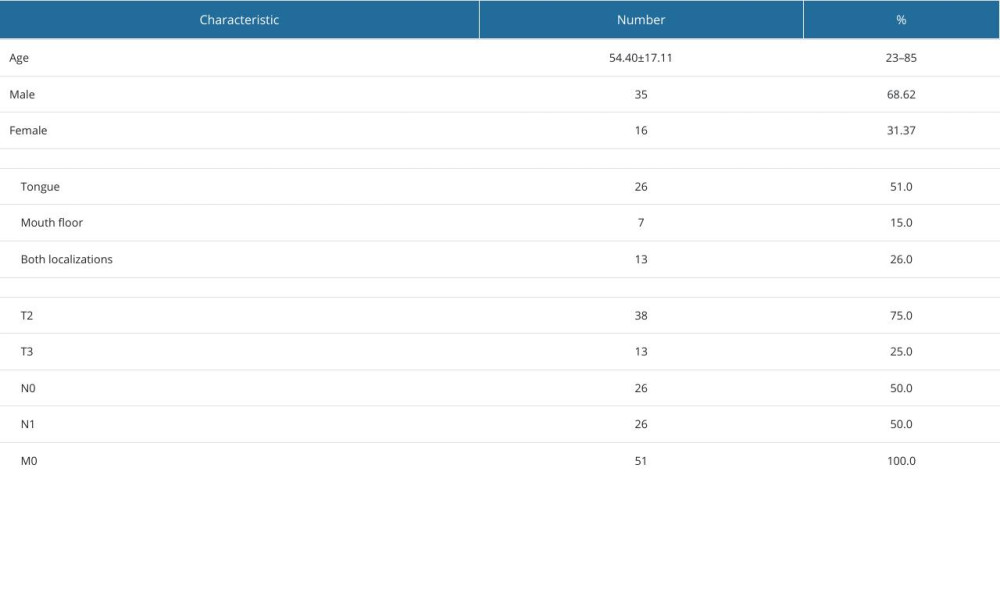 Table 1. Basic demographic and clinical characteristics of patients.
Table 1. Basic demographic and clinical characteristics of patients. Table 2. Pre- and post-treatment body mass index (BMI), serum albumin (ALB), prognostic nutritional index (PNI), and nutritional risk index (NRI) values.
Table 2. Pre- and post-treatment body mass index (BMI), serum albumin (ALB), prognostic nutritional index (PNI), and nutritional risk index (NRI) values.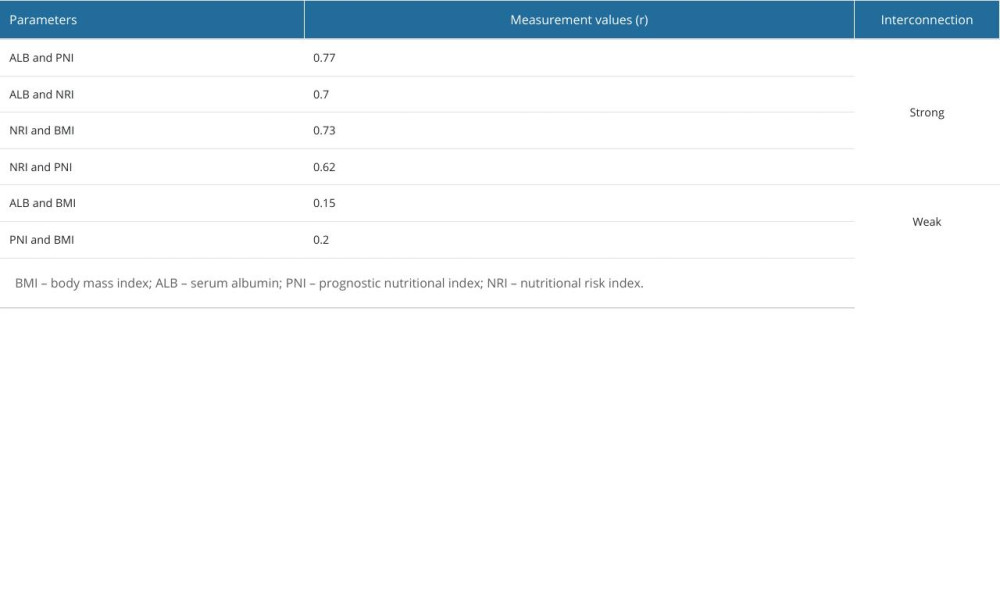 Table 3. Cox multivariate regression analysis between the examined parameters.
Table 3. Cox multivariate regression analysis between the examined parameters.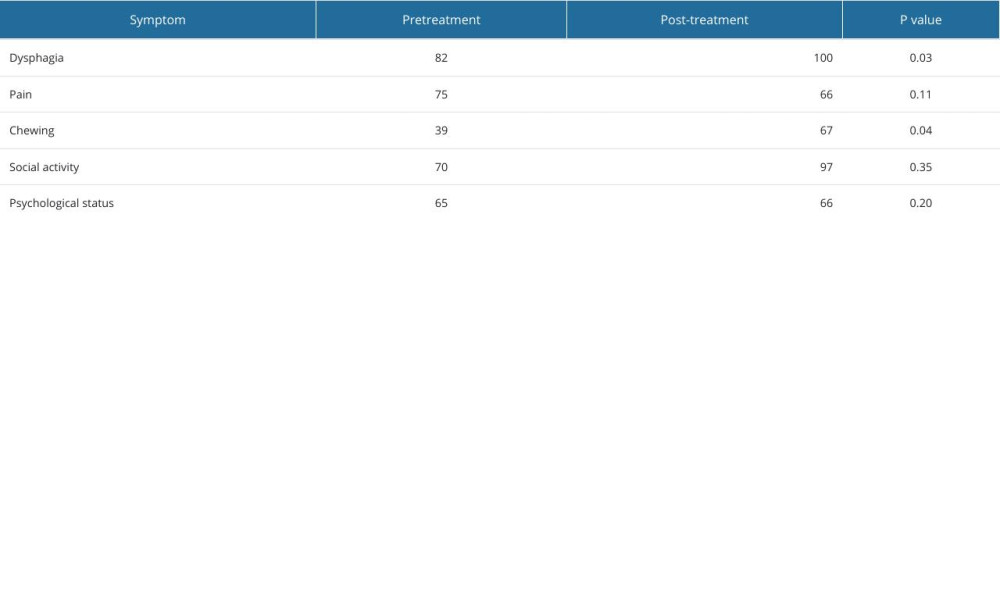 Table 4. Frequency of pretreatment and post-treatment quality of life parameters.
Table 4. Frequency of pretreatment and post-treatment quality of life parameters. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








