04 September 2020: Clinical Research
Clinical Characteristics and Outcomes of Patients with Severe COVID-19 and Chronic Obstructive Pulmonary Disease (COPD)
Yuanzhou He1BCG, Min Xie1DE, Jianping Zhao1CF, Xiansheng Liu1A*DOI: 10.12659/MSM.927212
Med Sci Monit 2020; 26:e927212
Abstract
BACKGROUND: The rapid worldwide spread of the coronavirus disease 2019 (COVID-19) epidemic has placed patients with pre-existing conditions at risk of severe morbidity and mortality. The present study investigated the clinical characteristics and outcomes of patients with severe COVID-19 and chronic obstructive pulmonary disease (COPD).
MATERIAL AND METHODS: This study enrolled 336 consecutive patients with confirmed severe COVID-19, including 28 diagnosed with COPD, from January 20, 2020, to April 1, 2020. Demographic data, symptoms, laboratory values, comorbidities, and clinical results were measured and compared in survivors and non-survivors.
RESULTS: Patients with severe COVID-19 and COPD were older than those without COPD. The proportions of men, of patients admitted to the intensive care unit (ICU) and of those requiring invasive ventilation were significantly higher in patients with than without COPD. Leukocyte and neutrophil counts, as well as the concentrations of NT-proBNP, hemoglobin, D-dimer, hsCRP, ferritin, IL-2R, TNF-α and procalcitonin were higher, whereas lymphocyte and monocyte counts were lower, in patients with than without COPD. Of the 28 patients with COPD, 22 (78.6%) died, a rate significantly higher than in patients without COPD (36.0%). A comparison of surviving and non-surviving patients with severe COVID-19 and COPD showed that those who died had a longer history of COPD, more fatigue, and a higher ICU occupancy rate, but a shorter average hospital stay, than those who survived.
CONCLUSIONS: COPD increases the risks of death and negative outcomes in patients with severe COVID-19.
Keywords: COVID-19, Outcome Assessment (Health Care), Pulmonary Disease, Chronic Obstructive, Age Distribution, Betacoronavirus, COVID-19, Cardiovascular Diseases, Comorbidity, Coronavirus Infections, Critical Care, Diabetes Mellitus, Fatigue, Length of Stay, Neoplasms, Pandemics, Pneumonia, Viral, Renal Insufficiency, Chronic, Respiration, Artificial, SARS-CoV-2, Sex Distribution, Survivors
Background
Since December 2019, the sudden outbreak of coronavirus disease 2019 (COVID-19) has become a prominent public health emergency worldwide, with severe negative effects, including high death rates and major economic disruptions [1]. As of May 1, 2020, 215 countries and regions had reported cases of viral infection, with over 3.2 million confirmed cases and over 234 000 deaths due to COVID-19 worldwide [2]. Factors associated with the risks of severe disease and death include older age, male sex, smoking, and comorbidities [3].
Chronic obstructive pulmonary disease (COPD) is common in China, estimated in 2020 to affect 13.7% of individuals aged >40 years [4]. Most patients affected by this disease are elderly men who have smoked for a long time. COPD is often associated with other systemic diseases and can lead to disordered pulmonary ventilation and even ventilation dysfunction. COPD can therefore increase the risk of infection and further complicate the treatment of patients with severe pulmonary infections. These findings suggested that COPD may increase the risks of severe COVID-19 infection and death.
The most common comorbidities associated with poor prognosis in patients with COVID-19 include hypertension, diabetes, heart disease, respiratory disease, pregnancy, kidney disease, and malignancy [5]. To date, however, less is known about the relationship between clinical presentation and prognosis in patients with severe COVID-19 and COPD [6]. The present study therefore analyzed the clinical characteristics of patients with severe COVID-19 and COPD and determined the relationship between COPD and the prognosis of patients with severe COVID-19.
Material and Methods
ETHICS STATEMENT:
The study was carried out in strict compliance with the provisions of the Declaration of Helsinki and was approved by the Tongji Medical College Ethics Committee at Tongji Hospital and the Huazhong University of Science and Technology Committee. All the patients provided oral informed consent.
STUDY DESIGN AND POPULATION:
This study included all patients hospitalized with severe COVID-19 at Tongji Hospital, Wuhan, China, from January 20, 2020, to April 10, 2020. Severe COVID-19 was defined as positivity for SARS-CoV-2 nucleic acid by real-time PCR or positivity for SARS-CoV-2-specific IgM and IgG antibodies and at least one of the following manifestations: respiratory rate (RR) ≥30/min, oxygen saturation ≤93% in a resting state, PaO2/FiO2 ≤300 mmHg, pulmonary imaging (CT/DR) showing significant progression >50% within 24 to 48 hours, respiratory failure requiring mechanical ventilation, shock, or admission to the Intensive Care Unit (ICU) for failure of other organs [7]. Patients with a previous history of COPD were defined as those with a long history of smoking, a diagnosis of COPD at our hospital, and treatment with inhaled drugs.
DATA COLLECTION:
Data collected from the medical records of each patient included age, sex, duration of COPD, treatment for COPD, comorbidities, and symptoms that included fever, sputum, dyspnea, cough, fatigue, chest pain, nausea, vomiting, and diarrhea. Laboratory parameters included routine blood tests; tests of liver, renal, and blood coagulation function; and concentrations of brain natriuretic peptide, troponin I, interleukin 2 receptor, C-reactive protein, procalcitonin, interleukin 6, interleukin 8, interleukin 10, and tumor necrosis factor-α. Also recorded were sepsis-related organ failure assessment (SOFA) score [8], patient outcomes, and length of stay in the hospital.
STATISTICAL ANALYSIS:
Because the incidence and prevalence of COVID-19 in COPD patients were unknown, sample size could not be calculated prior to the study. Normally distributed continuous variables were reported as the mean±SEM and compared by independent
Results
This study enrolled 336 consecutively hospitalized patients with severe COVID-19, including 28 with COPD. The overall median age was 65 (50-77) years but was significantly higher in patients with than without COPD (71 [63–79] years
The most common symptoms of severe COVID-19 were fever (88.7%), cough (76.0%), dyspnea (60.4%), fatigue (47.9%), and expectoration (28.9%). Cough, expectoration, dyspnea, and fatigue were more common in patients with COPD than in those without COPD. Other symptoms, including diarrhea (27.7%), nausea (5.7%), vomiting (3.6%), and chest pain (2.4%), as well as SOFA scores, did not differ significantly in these 2 groups. Of the 28 patients with severe COVID-19 and COPD, 19 (67.9%) were admitted to the ICU, a rate significantly higher than in patients without COPD (45.4%). All patients with COPD used glucocorticoids, compared with only 54.5% of those without COPD. Similarly, the utilization rates of invasive ventilation were higher in patients with (67.9%) COPD than in those without (38.0%) COPD. In addition, median hospital stay (11 [6–14] days
At admission, COPD patients had higher leukocyte (8.24×109/L
Of the 336 patients with severe COVID-19, 133 (39.6%) died. Compared with survivors, non-survivors were older (69 [57–80]
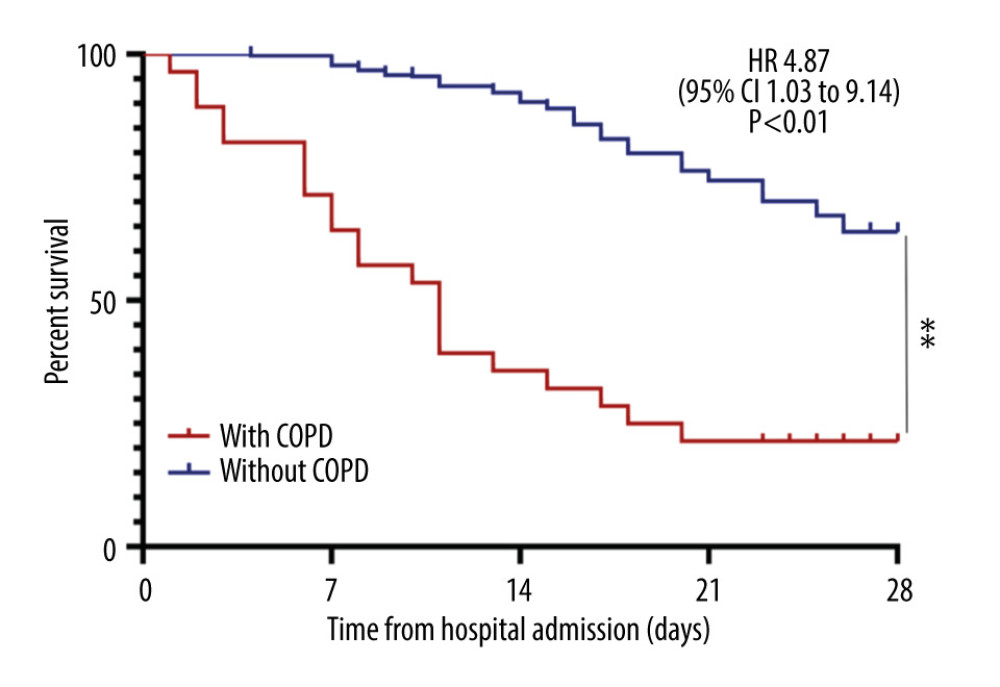
Of the 28 patients with severe COVID-19 and COPD, 22 (78.6%) died. Kaplan-Meier analysis showed that the overall survival rate was worse in severe COVID-19 patients with than without COPD (HR 4.87; 95% CI 1.03 to 9.14,
A comparison of survivors and non-survivors in the group with severe COVID-19 and COPD showed that those who died were significantly more likely to be men (
Discussion
Despite the widespread COVID-19 pandemic and the large numbers of infected patients, relatively little is known about the clinical course in patients with severe COVID-19 and COPD [9]. Of the 336 patients with severe COVID-19 included in this study, only 28 (8.3%) had COPD. These patients were older, had more severe inflammation, and were more prone to bacterial infection than patients with severe COVID-19 without COPD. Furthermore, Kaplan-Meier analysis demonstrated that overall survival was significantly lower in severe COVID-19 patients with COPD than in those without COPD. Our results showed that COPD was strongly associated with poor prognosis and with adverse clinical outcomes such as ICU admission, glucocorticoid use, invasive mechanical ventilation, and death. Comparisons of survivors and non-survivors with severe COVID-19 and COPD showed that non-survivors were older, were more likely to be men and were more likely to be admitted to the ICU than survivors.
Most COPD patients in China are men with a long history of smoking. In addition, more COVID-19 patients are male, as SARS-CoV-2 infection is through the ACE2 receptor, which is expressed at almost 3-fold higher levels in men than in women [10–12]. Long-term exposure to smoke damages the airway intima and induces the proliferation of airway smooth muscle cells, airway remodeling, disordered pulmonary function, and even ventilation disorders [13]. SARS-CoV-2 infection exacerbates previous lung function injury, significantly increasing the rates of ventilator use and ICU admission. Glucocorticoids are widely used to relieve airway inflammation, especially in severely ill patients [14]. However, anatomically small airways are chronically damaged in COPD patients. Because this damage is usually combined with bronchiectasis and obstruction of airway sputum removal, the small airways are more likely to be infected with bacteria, even with extensively drug-resistant bacteria, exacerbating the original severe pulmonary infection [15]. Together, these factors contribute to a high risk of adverse outcomes in patients with severe COVID-19 and COPD.
Cardiovascular and cerebrovascular diseases are more likely to be present in severe COVID-19 patients with than without COPD. These conditions may be due to long-term hypoxia, chronic inflammation, and other factors leading to vascular endothelial injury [16]. Although the clinical features of the 2 groups in the present study were generally similar, cough, expectoration, dyspnea, and fatigue occurred more frequently in patients with than without COPD. However, because of the small sample size, the differences were not statistically significant.
Laboratory test results showed that lymphocyte and monocyte counts were significantly lower, whereas leukocyte and neutrophil counts, as well as hemoglobin and procalcitonin (PCT) levels, were significantly higher, in patients with than without COPD. These results suggested that bacterial infection may have occurred after viral infection. However, the higher hemoglobin concentration in patients with COPD may have been due to a lack of oxygen. In addition, we found that markers of inflammation, such as hsCRP, ferritin, IL-2R, and TNF-α, were higher in patients with than without COPD, as were the rates of coagulation disorders and myocardial injuries. A comparison of surviving and non-surviving patients with severe COVID-19 and COPD found that leukocyte counts, neutrophil counts, and procalcitonin levels were higher, whereas lymphocyte and monocyte counts were lower, in non-survivors. Moreover, there was greater damage to myocardial, hepatic, and renal functions in non-survivors than in survivors. These results indicate that the degree of inflammation is greater in severe COVID-19 patients with than without COPD and that the degree of inflammation is closely related to patient prognosis.
This study has several limitations. First, it was a single-center, retrospective study in a relatively small number of patients, which made it difficult to accurately assess various risk factors using a multifactor regression model. Second, the diagnosis of COPD was based on patient history, not on objective analysis of lung function. Third, this study focused on patients with early-stage COVID-19, indicating the need for studies in the later stages of this disease.
Conclusions
These results indicate that severe COVID-19 patients with COPD have a higher prevalence of cardiovascular and cerebrovascular diseases, are more likely to receive mechanical ventilation and to be treated in the ICU, and have a higher mortality rate than severe COVID-19 patients without COPD. These results also suggest that, in severe COVID-19 patients, COPD is a high risk factor for poor prognosis. Therefore, COPD patients should be more vigilant to prevent infection with COVID-19. Larger studies with longer follow-up durations are needed to confirm these findings.
Tables
Table 1. Clinical features of severe COVID-19 patients with and without COPD.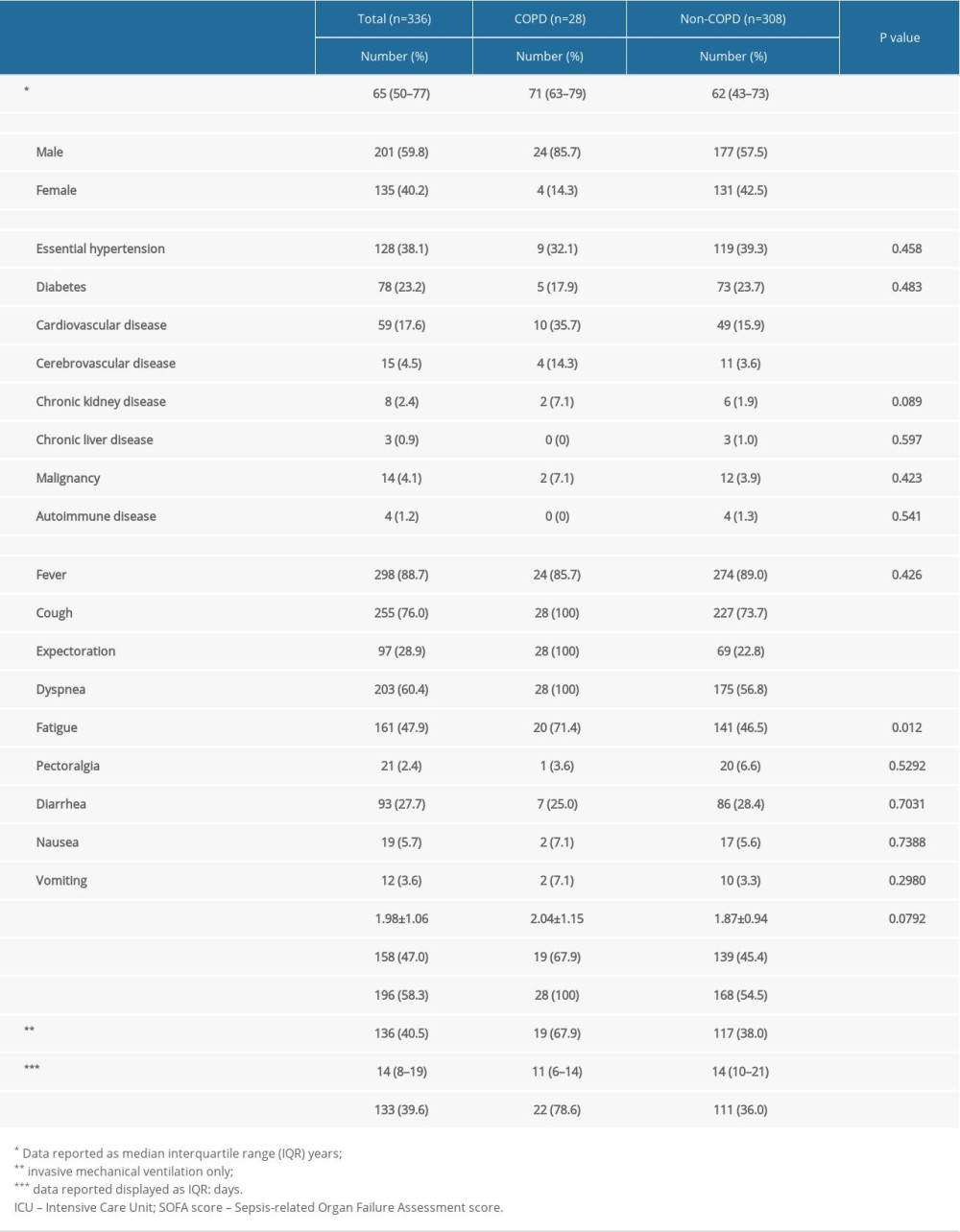 Table 2. Laboratory results of severe COVID-19 patients with and without COPD.
Table 2. Laboratory results of severe COVID-19 patients with and without COPD.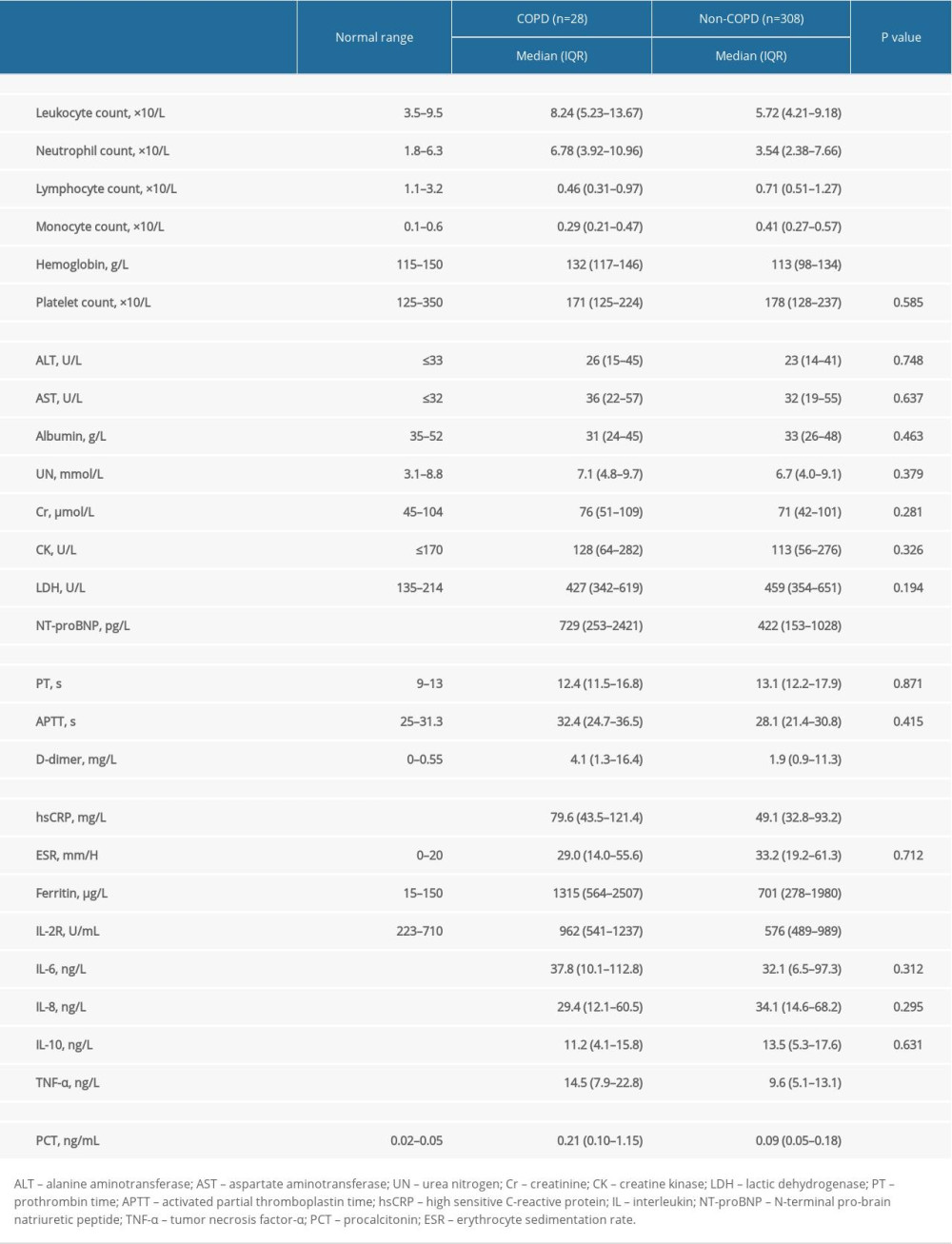 Table 3. Baseline characteristics of survivors and non-survivors with severe COVID-19 patients.
Table 3. Baseline characteristics of survivors and non-survivors with severe COVID-19 patients.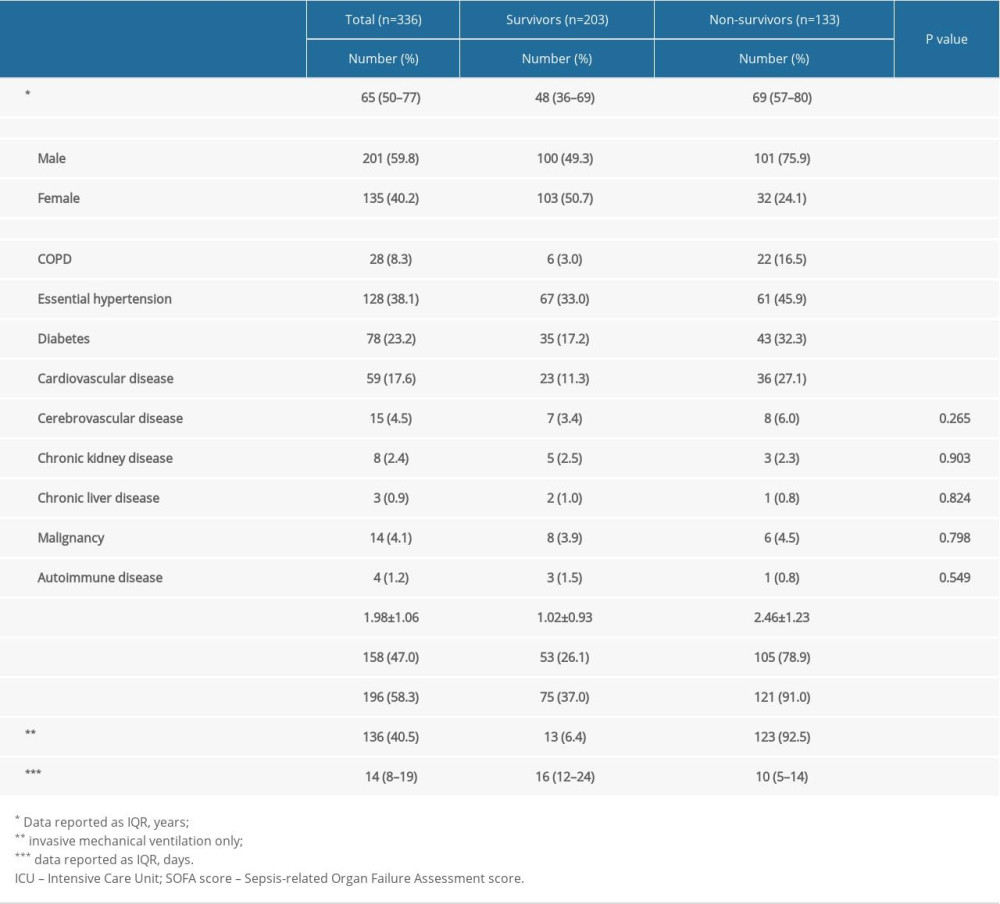 Table 4. Clinical features of survivors and non-survivors with severe COVID-19 and COPD.
Table 4. Clinical features of survivors and non-survivors with severe COVID-19 and COPD.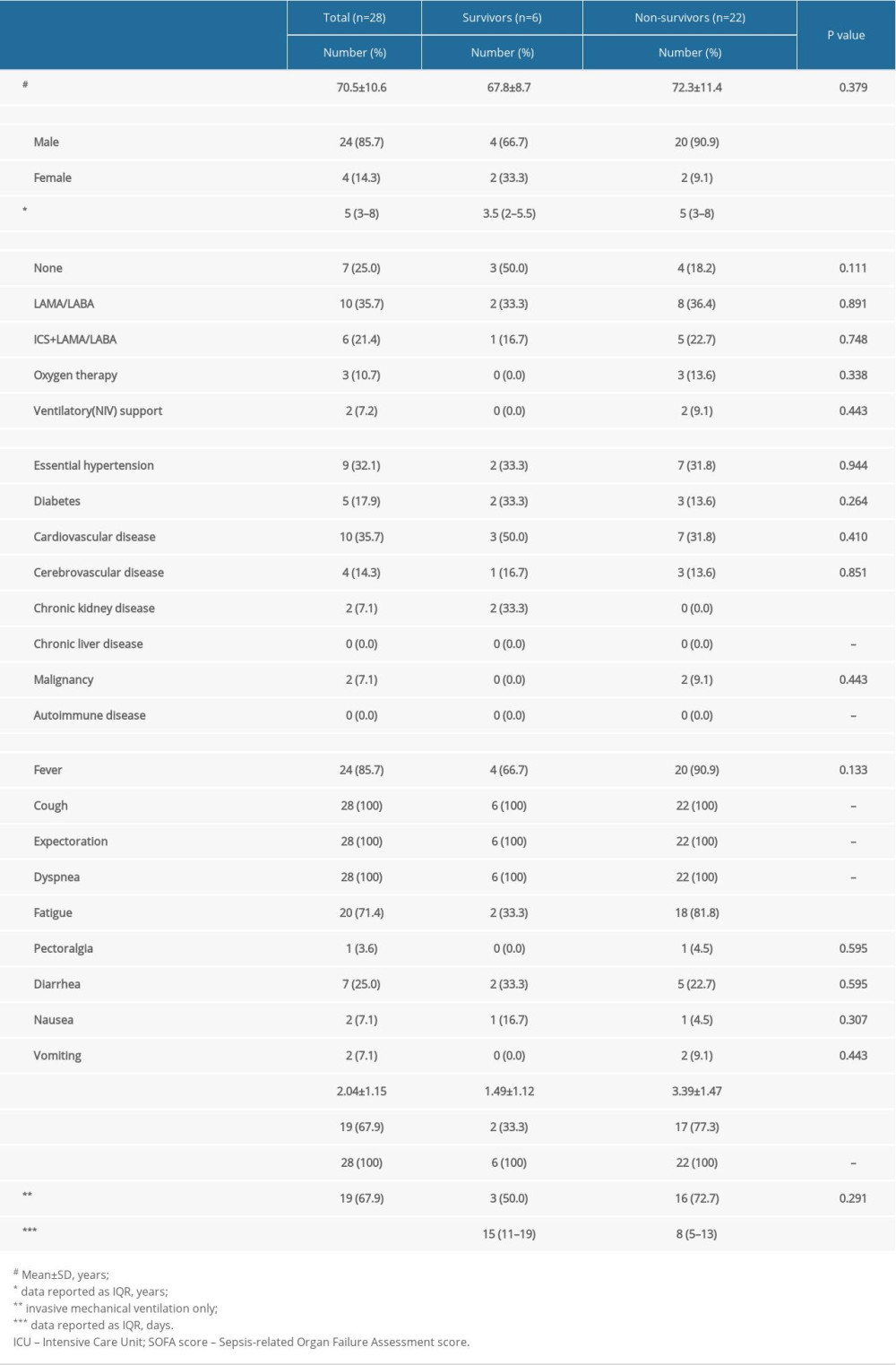 Table 5. Laboratory findings of survivors and non-survivors with severe COVID-19 and COPD.
Table 5. Laboratory findings of survivors and non-survivors with severe COVID-19 and COPD.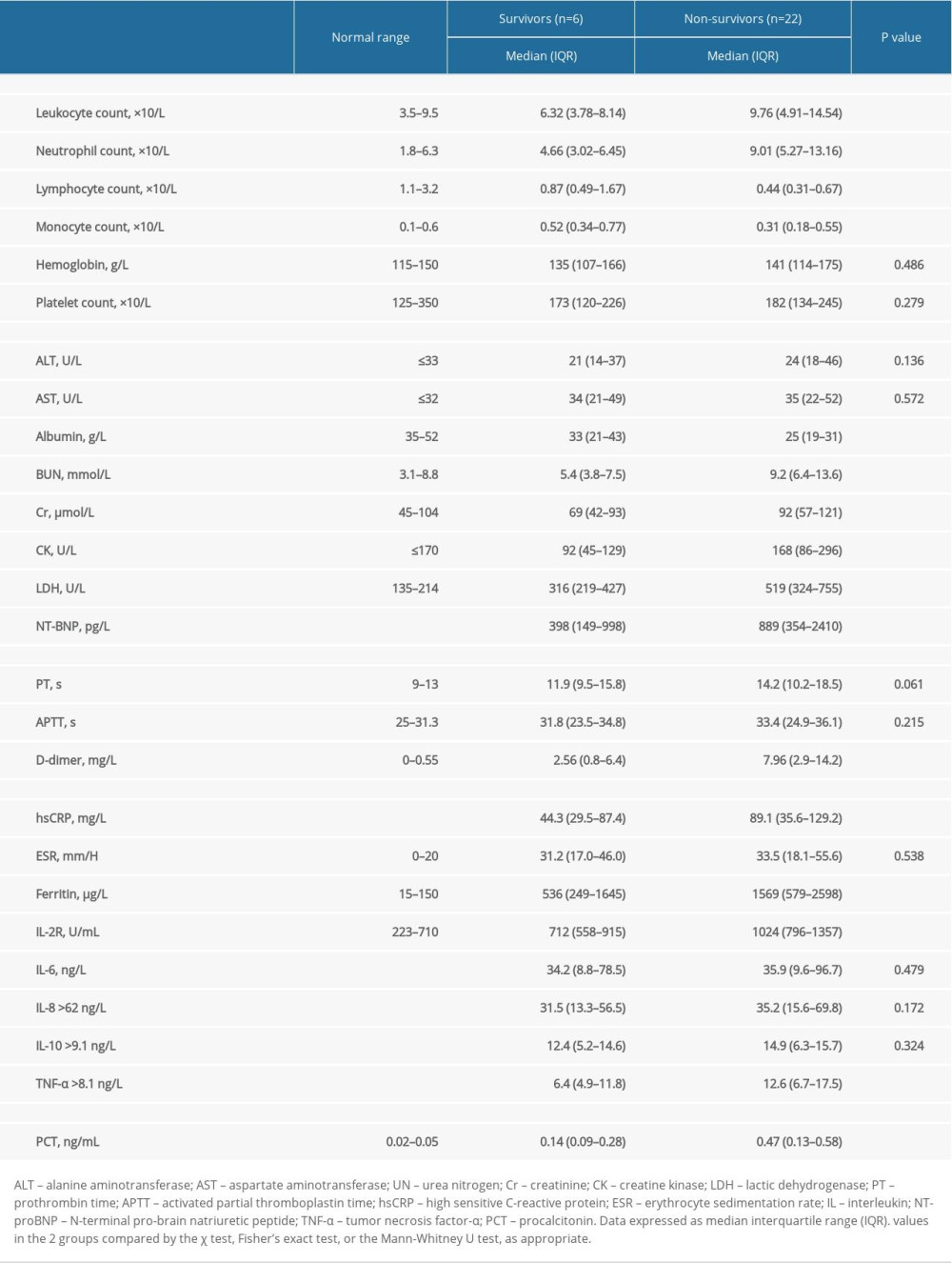
References
1. : WHO main website, 2020 https://www.who.int
2. World Health Organization: Novel Coronavirus (2019-nCoV) situation reports, 2020 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
3. Horowitz RI, Freeman PR, Three novel prevention, diagnostic, and treatment options for COVID-19 urgently necessitating controlled randomized trials: Med Hypotheses, 2020; 143; 109851
4. Wagner PD, Viegi G, Luna CM, Major causes of death in China: N Engl J Med, 2006; 354(8); 874-76
5. Ji HL, Zhao R, Matalon S, Matthay MA, Elevated plasmin(ogen) as a common risk factor for COVID-19 susceptibility: Physiol Rev, 2020; 100(3); 1065-75
6. Halpin DMG, Faner R, Sibila O, Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection?: Lancet Respir Med, 2020; 8(5); 436-38
7. World Health Organization: Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance https://www.who.int/internal-publications-detail/clinical-managementof-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected
8. Raith EP, Udy AA, Bailey MAustralian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE), Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit: JAMA, 2017; 317(3); 290-300
9. Zhu N, Zhang D, Wang WChina Novel Coronavirus Investigation and Research Team, A novel coronavirus from patients with pneumonia in China, 2019: N Engl J Med, 2020; 382(8); 727-33
10. Thachil J, Tang N, Gando S, ISTH interim guidance on recognition and management of coagulopathy in COVID-19: J Thromb Haemost, 2020; 18(5); 1023-26
11. Wang L, He W, Yu X, Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up: J Infect, 2020; 80(6); 639-45
12. Lu R, Zhao X, Li J, Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding: Lancet, 2020; 395(10224); 565-74
13. López-Campos JL, Tan W, Soriano JB, Global burden of COPD: Respirology, 2016; 21(1); 14-23
14. Mirza S, Clay RD, Koslow MA, Scanlon PD, COPD guidelines: A review of the 2018 GOLD report: Mayo Clin Proc, 2018; 93(10); 1488-502
15. Cui Y, Luo L, Li C, Long-term macrolide treatment for the prevention of acute exacerbations in COPD: A systematic review and meta-analysis: Int J Chron Obstruct Pulmon Dis, 2018; 13; 3813-29
16. Deng F, Wang S, Xu R, Endothelial microvesicles in hypoxic hypoxia diseases: J Cell Mol Med, 2018; 22(8); 3708-18
Tables
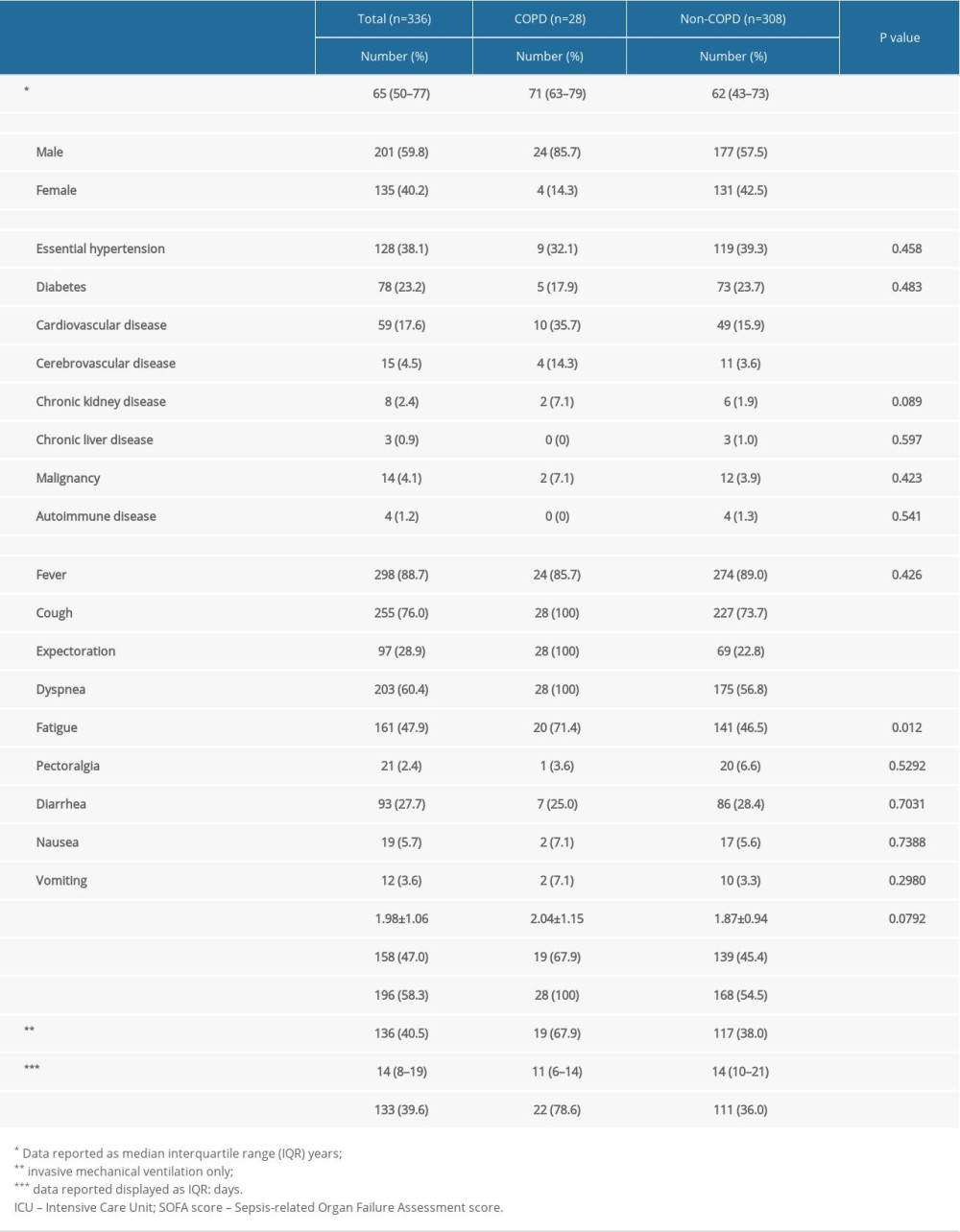 Table 1. Clinical features of severe COVID-19 patients with and without COPD.
Table 1. Clinical features of severe COVID-19 patients with and without COPD.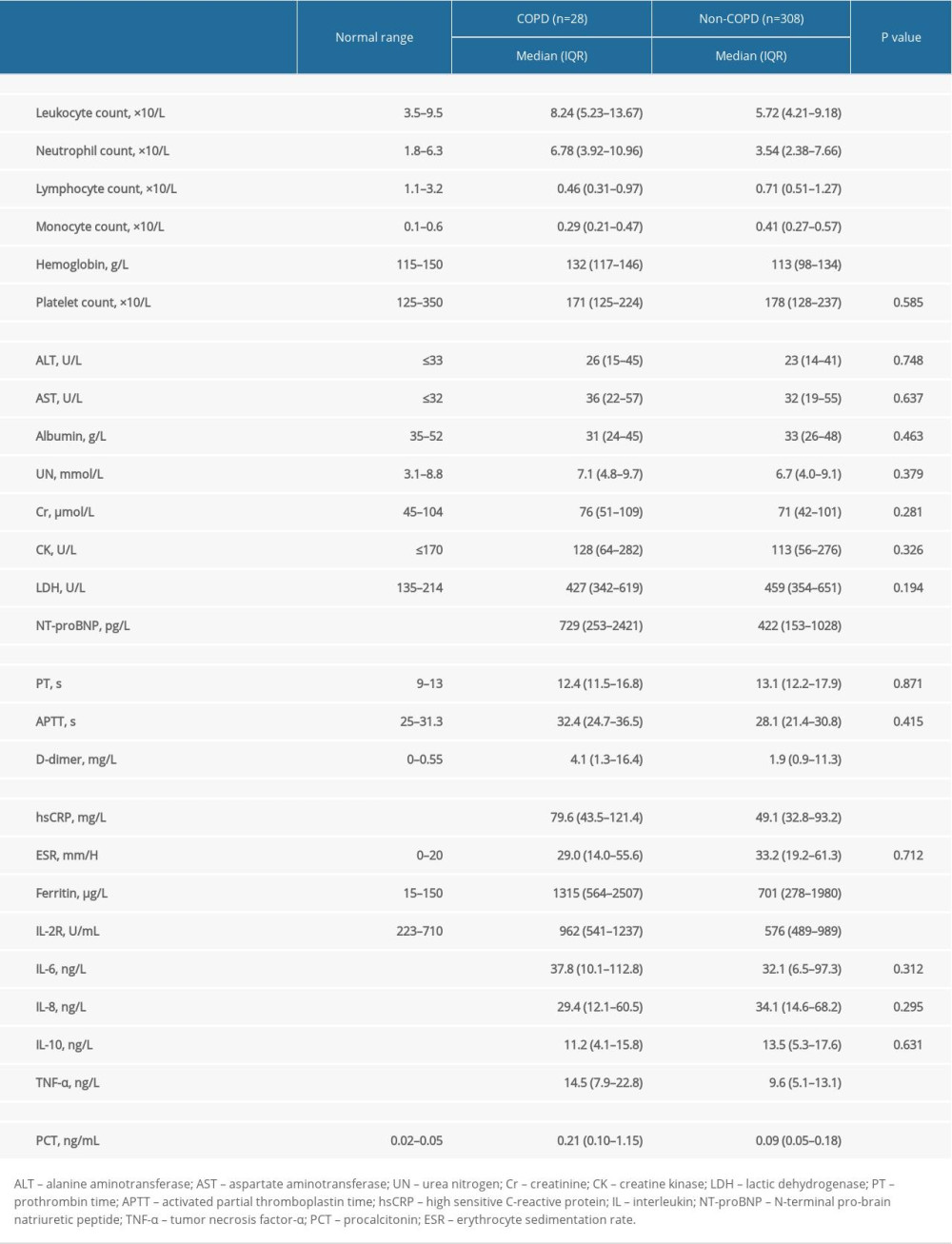 Table 2. Laboratory results of severe COVID-19 patients with and without COPD.
Table 2. Laboratory results of severe COVID-19 patients with and without COPD.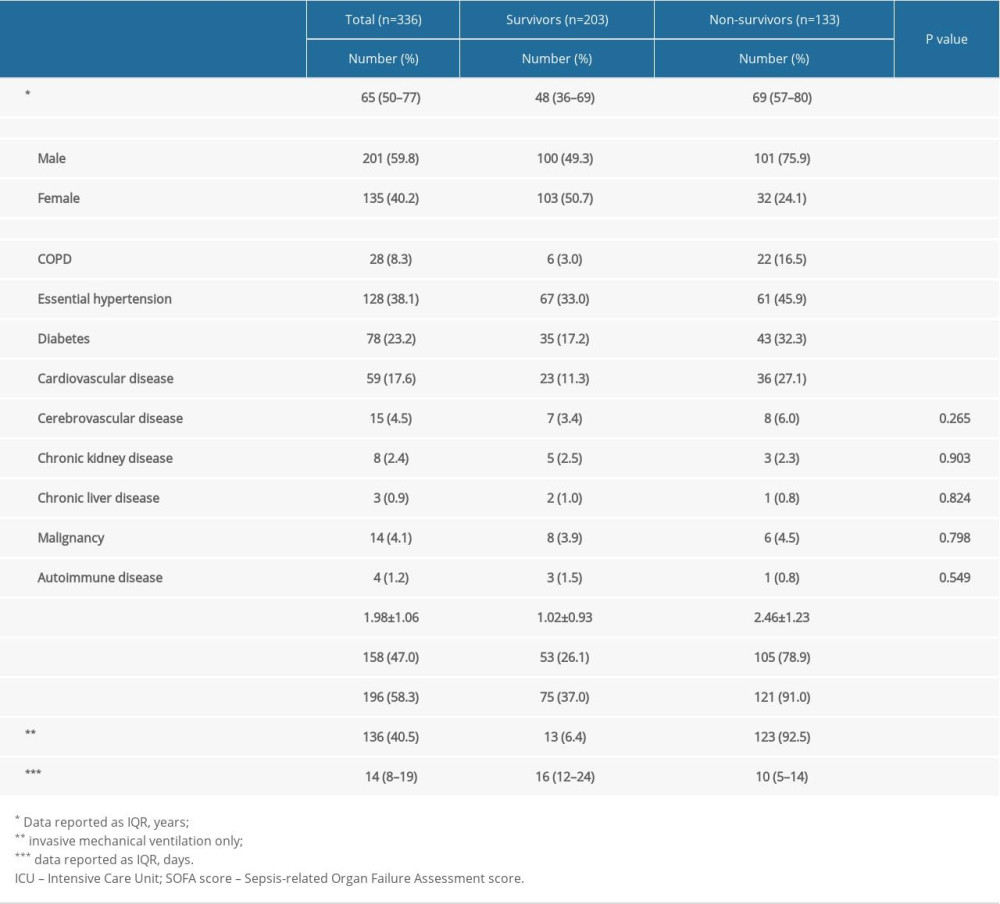 Table 3. Baseline characteristics of survivors and non-survivors with severe COVID-19 patients.
Table 3. Baseline characteristics of survivors and non-survivors with severe COVID-19 patients.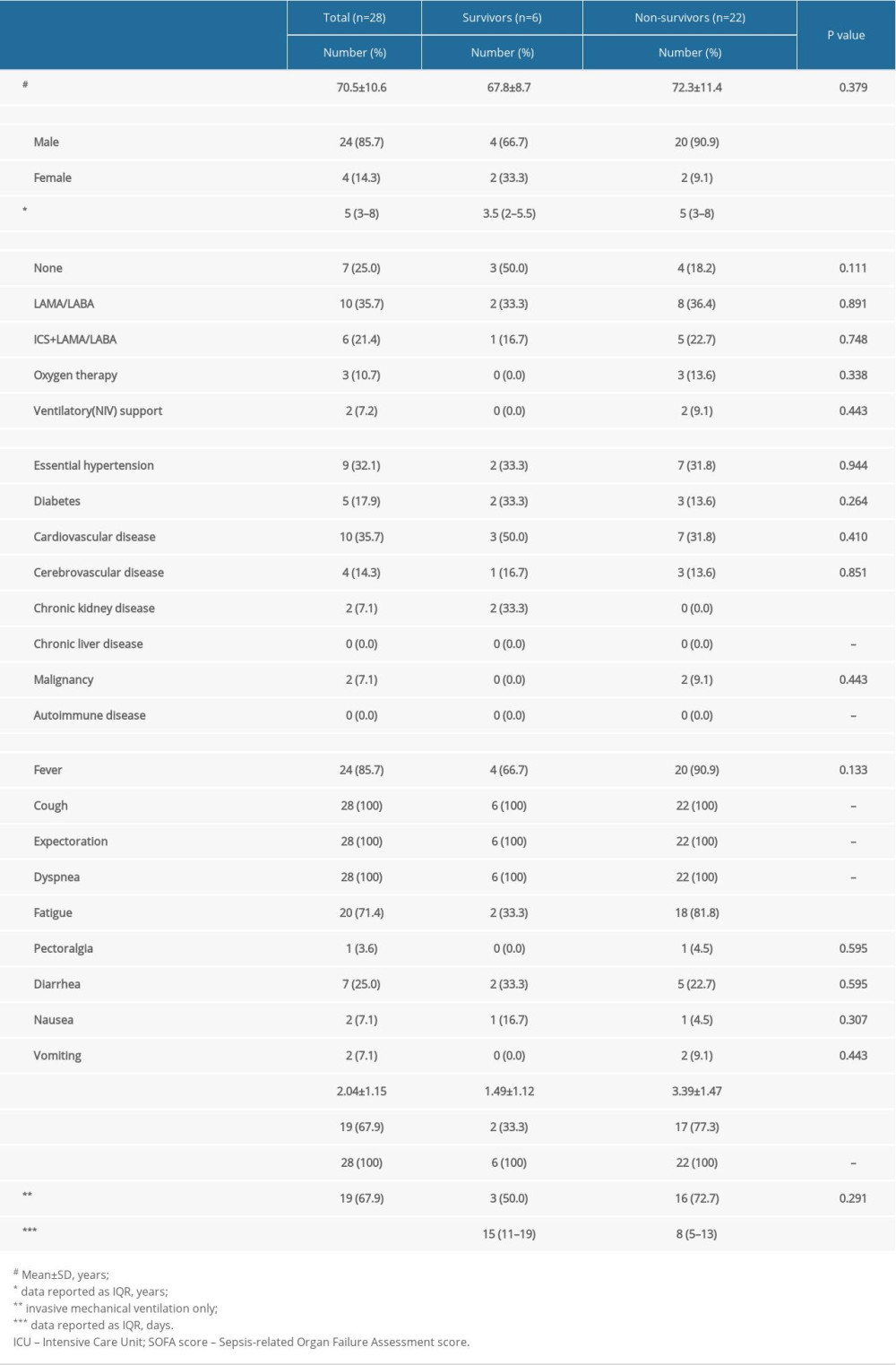 Table 4. Clinical features of survivors and non-survivors with severe COVID-19 and COPD.
Table 4. Clinical features of survivors and non-survivors with severe COVID-19 and COPD.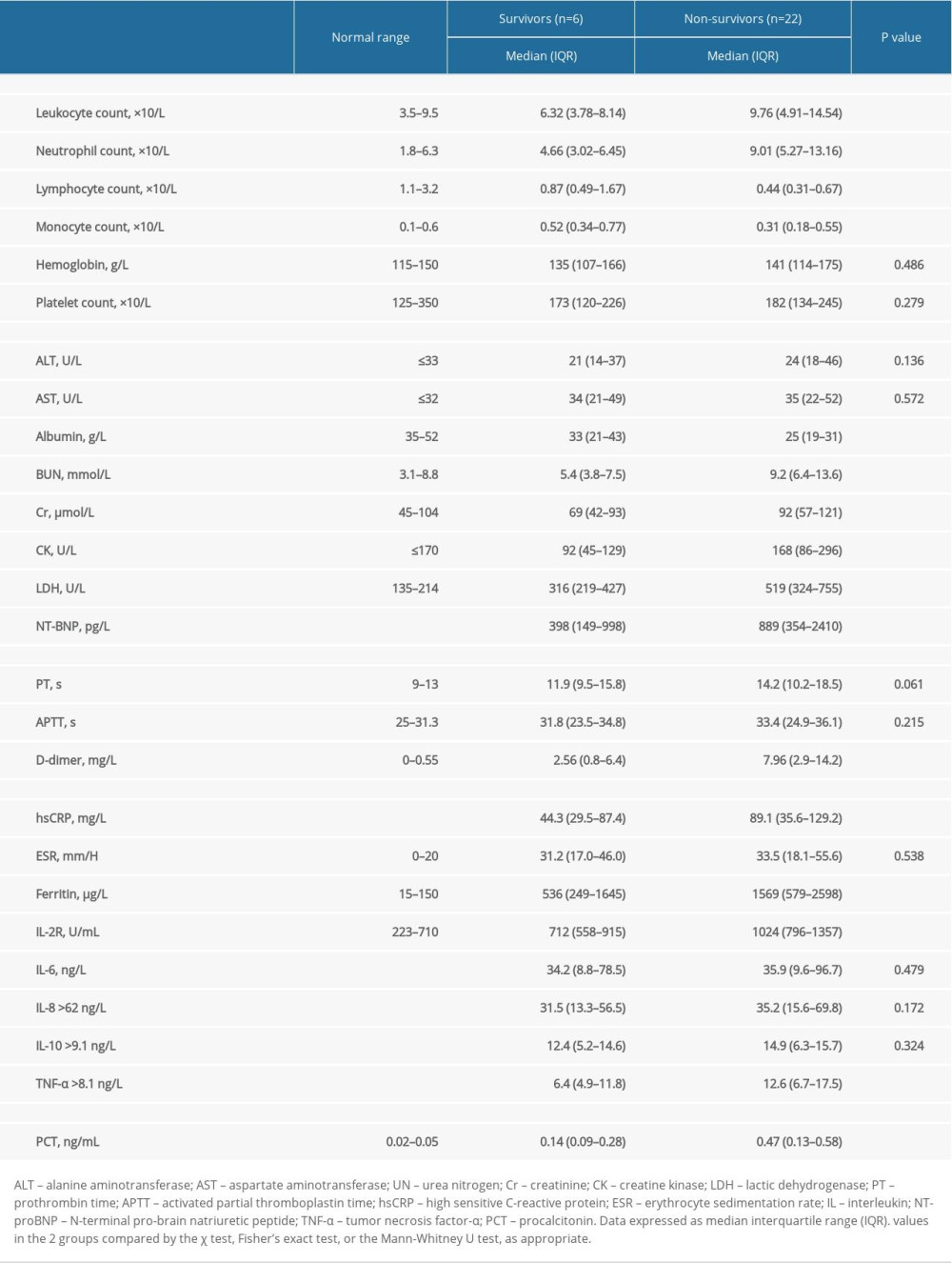 Table 5. Laboratory findings of survivors and non-survivors with severe COVID-19 and COPD.
Table 5. Laboratory findings of survivors and non-survivors with severe COVID-19 and COPD.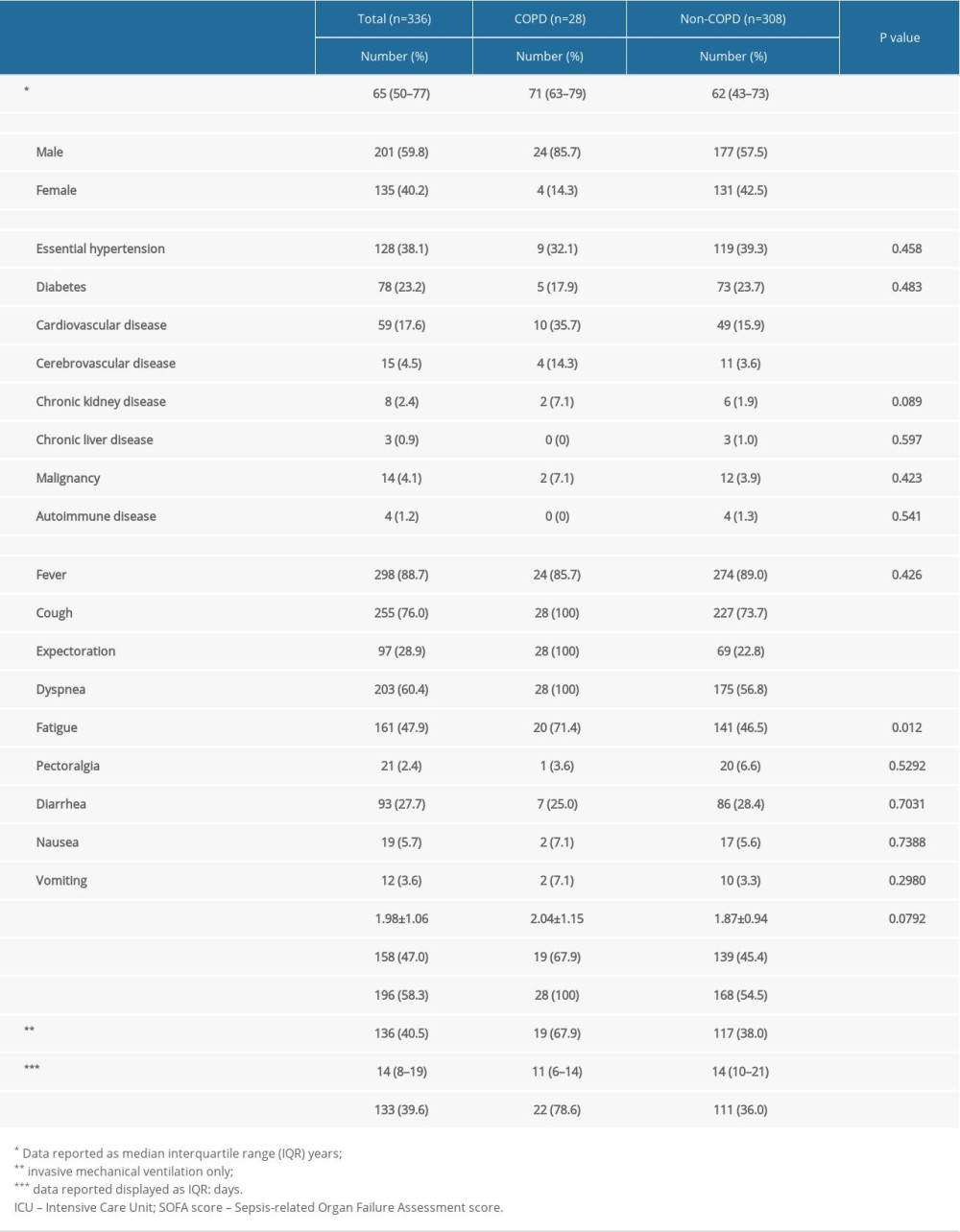 Table 1. Clinical features of severe COVID-19 patients with and without COPD.
Table 1. Clinical features of severe COVID-19 patients with and without COPD.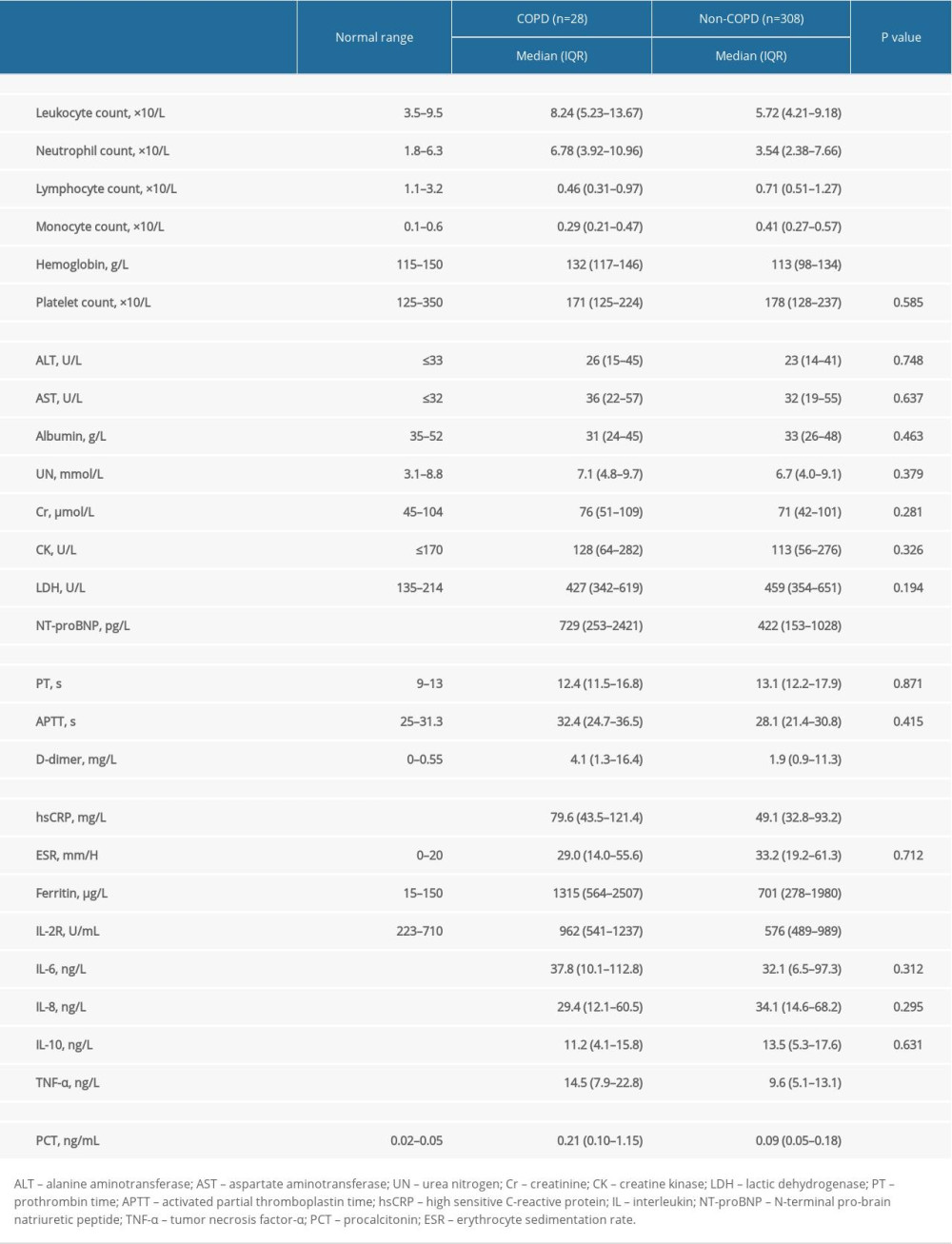 Table 2. Laboratory results of severe COVID-19 patients with and without COPD.
Table 2. Laboratory results of severe COVID-19 patients with and without COPD.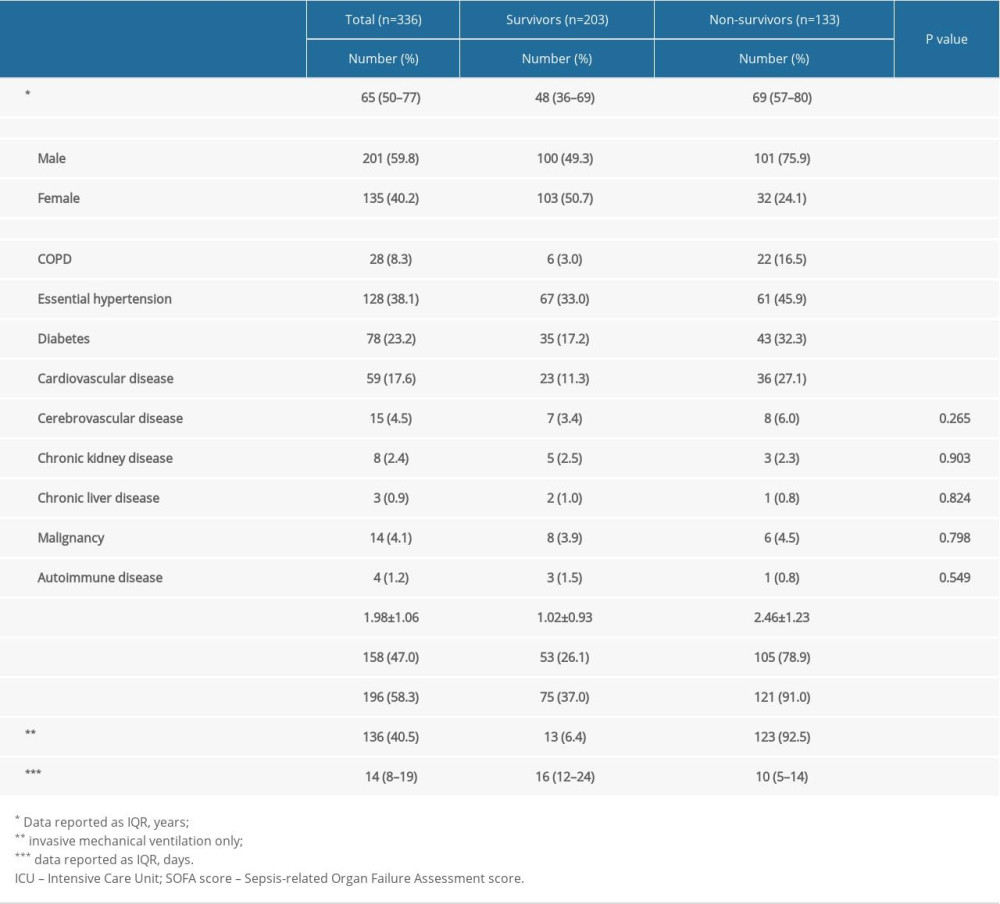 Table 3. Baseline characteristics of survivors and non-survivors with severe COVID-19 patients.
Table 3. Baseline characteristics of survivors and non-survivors with severe COVID-19 patients.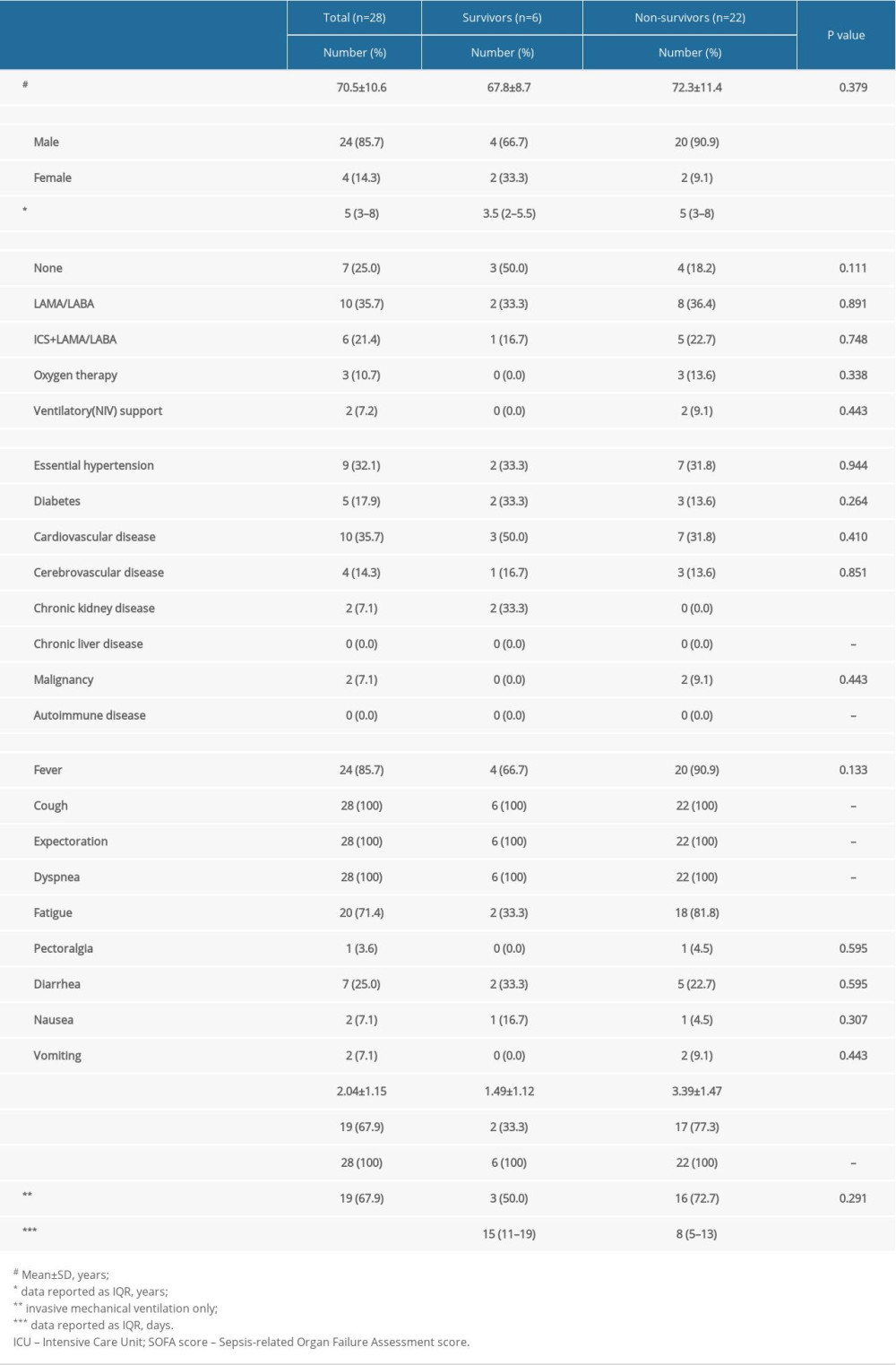 Table 4. Clinical features of survivors and non-survivors with severe COVID-19 and COPD.
Table 4. Clinical features of survivors and non-survivors with severe COVID-19 and COPD.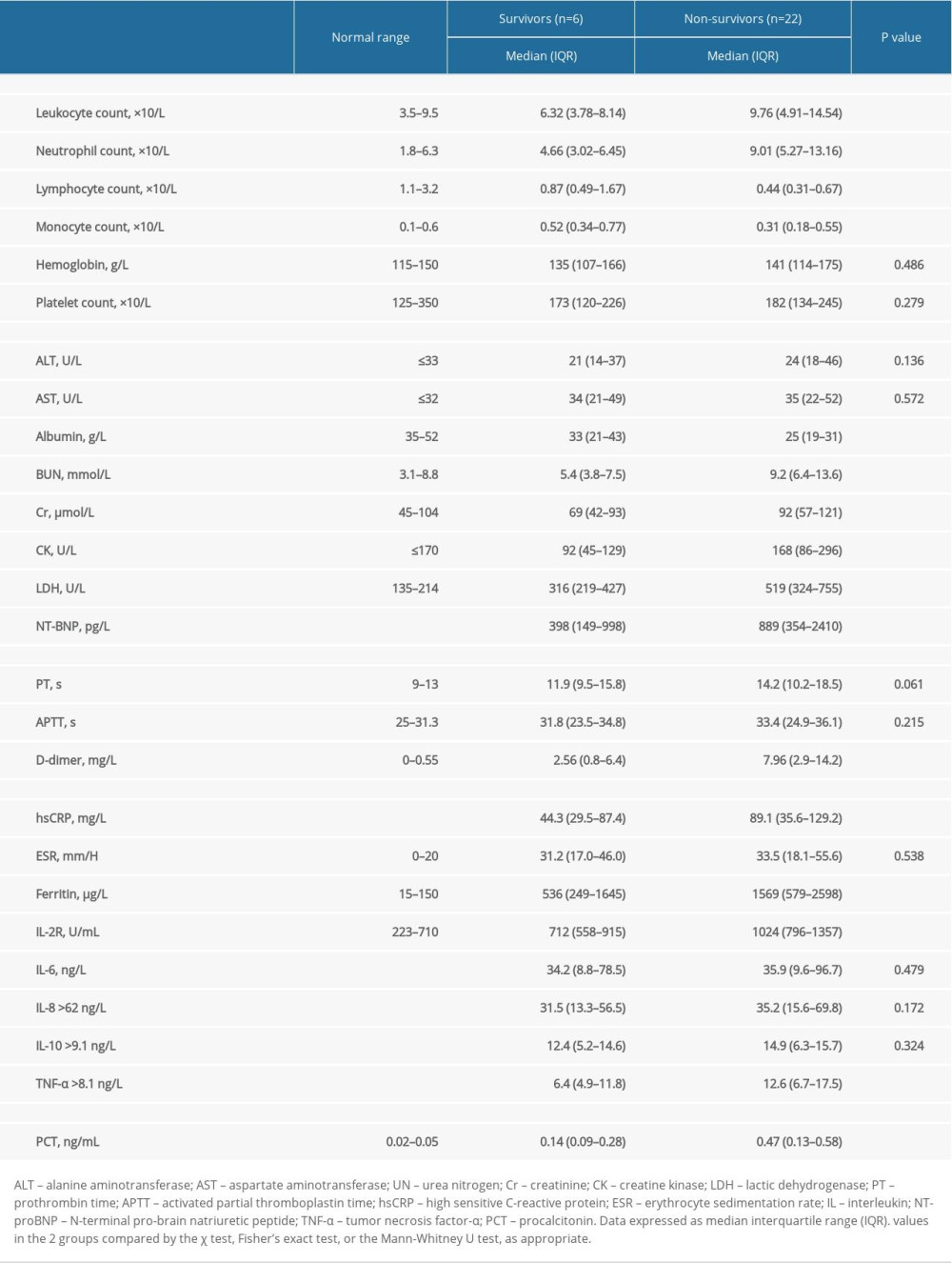 Table 5. Laboratory findings of survivors and non-survivors with severe COVID-19 and COPD.
Table 5. Laboratory findings of survivors and non-survivors with severe COVID-19 and COPD. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952