15 August 2023: Clinical Research
Risk Factors and Causes of Reoperation in Lumbar Disc Herniation Patients after Percutaneous Endoscopic Lumbar Discectomy: A Retrospective Case Series with a Minimum 2-Year Follow-Up
Tao Tang1BCDE, Jiahao Liu2ACD, Jian Cao2A, Dingwen He2AE, Xigao Cheng2AEG, Shuihua Xie1CDEFG*DOI: 10.12659/MSM.939844
Med Sci Monit 2023; 29:e939844
Abstract
BACKGROUND: Percutaneous endoscopic lumbar discectomy (PELD) has gained popularity as a minimally invasive surgery for treating lumbar disc herniation. However, there is limited research focusing on the reoperation rate and its associated factors. This study aims to investigate the rate of reoperation and identify the causes and risk factors for reoperation after PELD.
MATERIAL AND METHODS: We conducted a retrospective analysis of patients who underwent PELD (interlaminar and transforaminal approaches) at our hospital from November 2016 to May 2020. A matched case-control design was employed to identify relevant risk factors for reoperation, with a matching ratio of 1:3. Clinical characteristics and radiological parameters were compared, and univariate analysis was performed using independent samples t-test and chi-squared test.
RESULTS: Among the 435 patients included in the study, the reoperation rate for those with a minimum 2-year follow-up was 6.2% (27/435). The causes of reoperation and their respective rates were as follows: recurrence of lumbar disc herniation (3.2%, 14/435), incomplete decompression (1.8%, 8/435), persistent low back pain (0.7%, 3/435), and postoperative infection (0.5%, 2/435). Univariate analysis revealed that age (P=0.015), Pfirrmann grade IV-V (P=0.017), and lack of active straight leg raise exercises (P=0.026) were significantly associated with reoperation. Multiple logistic regression analysis indicated that age (P=0.001), Pfirrmann grade IV-V (P=0.033), and lack of active straight leg raise exercises postoperatively (P=0.003) were independent risk factors for reoperation after PELD.
CONCLUSIONS: The primary cause of reoperation in lumbar disc herniation patients after PELD was recurrence of the herniation. Additionally, severe disc degeneration, older age, and lack of active straight leg raise exercises were identified as significant risk factors associated with an increased reoperation rate.
Keywords: Minimally Invasive Surgical Procedures, Recurrence, Reoperation, Risk Factors, Humans, Intervertebral Disc Displacement, Diskectomy, Percutaneous, Retrospective Studies, Follow-Up Studies, Lumbar Vertebrae, Diskectomy, endoscopy, Research Design, Treatment Outcome
Background
Percutaneous endoscopic lumbar discectomy (PELD) is a minimally invasive technique that can treat various types of lumbar disc herniation (LDH) [1,2]. Since the introduction of the percutaneous discectomy by Kambin in 1973, PELD has become more and more widely used in recent years [3]. Compared with open discectomy, the advantages of PELD include fast recovery, local anesthesia, mild tissue damage, favorable outcomes, and short hospital stay [2,4]. However, some previous studies have indicated that the learning curve of PELD is very steep and requires constant training of surgeons to overcome it, and PELD has a higher risk of recurrence than traditional discectomy [5–7]. For young and inexperienced spinal surgeons, the risk of surgical failure is higher and may require reoperation [5–7]. Although the PELD procedure is relatively complex, it is welcomed by patients with LDH and spinal surgeons because it retains the integrity of the posterior lumbar muscles and bony structures [8]. However, the rate, the reasons, and the risk factors for reoperation have not been fully reported in patients with LDH who underwent PELD. Therefore, the purpose of this study was to calculate the reoperation rate and elaborate on the common reasons for reoperation after PELD, and to identify the risk factors for reoperation after PELD. In addition, we present a series of cases who underwent reoperation.
Material and Methods
PATIENTS:
This study was a retrospective, observational case series. Based on the picture archiving and communication system (PACS) of our hospital, we retrospectively collected the data of 435 patients with LDH who underwent PELD (including the interlaminar approach and transforaminal approach) in our hospital from November 2016 to May 2020. The diagnosis of LDH was confirmed by the lumbar magnetic resonance imaging (MRI), computed tomography (CT), and X-ray. Follow-up methods include outpatient service and telephone survey.
The inclusion criteria were as follows:
The exclusion criteria included the following:
Out of 492 patients, 57 patients did not meet the study criteria. Ultimately, a total of 435 cases (229 men, 206 women, average age: 52.7±12.2, range, 18–88 years) were included in this study. Reoperation was defined as cases that underwent surgery again in the same segment [9].
ETHICS APPROVAL AND CONSENT TO PARTICIPATE:
This current study was conducted in accordance with the principles of the 1975 Helsinki Declaration revised in 2008. All of the protocols involving patients were approved by the Ethics Committee of the Second Affiliated Hospital of Nanchang University. All the patients signed the informed consent form before surgery.
STEP 1. ANESTHESIA AND POSITION:
All operations were performed by 2 spine surgery specialists with 5 years of experience in PELD. Patients were given non-steroidal anti-inflammatory and analgesic drugs (parecoxib sodium 40 mg) 30 minutes before surgery. Generally, 2 surgical approaches for PELD were selected according to the level of LDH: the transforaminal approach was applied for LDH located at L3–4 or L4–5, and the interlaminar approach was used for or LDH at L5-S1. Patients with the interlaminar approach were in prone position, while patients with the transforaminal approach were in lateral position. The PELD was performed under local anesthesia, and patients could communicate with the surgeon during the whole operation process to avoid injury to nerve roots.
STEP 2. PUNCTURE AND CHANNEL PLACEMENT:
After placing patients in the proper body position, we used C-arm X-ray to define the entry point before the puncture, an 18-G needle was introduced to anesthetize the path with 10 ml of 1% lidocaine. Then, the working channel was placed according to the standard spinal endoscopy system. If we found that the foraminal stenosis or the interlaminar space was narrowed during channel placement, we used a trephine to remove part of the superior articular process or lamina.
STEP 3. DECOMPRESSION AND SUTURED THE SKIN INCISION:
Next, the decompression was performed: after confirming the structure under a clear endoscope, we used various grasping forceps to remove the herniated intervertebral disc. Before the end of the operation, the passive straight-leg raise test was carried out to detect the effect of the operation, and patients were asked to cough loudly to check for any residual herniated disc that had not been removed. At the end of the procedure, the dural sac and nerve roots were freely mobilized, then 5 mg of dexamethasone was injected in the channel. The incision was closed with a single 3-0 nylon suture.
STEP 4. POSTOPERATIVE REHABILITATION:
After returning to the ward, the doctors taught the patients to perform active straight-leg raise exercises in a hospital bed, then asked the patients to stay in bed as much as possible for 1 month and to perform at least 100 active straight-leg raise exercises every day during the bedridden rehabilitation period after discharge.
DATA COLLECTION AND ASSESSMENT:
The collected clinical data and radiologic parameters of patients included age at index surgery, sex, body mass index (BMI), disease duration (months), surgery mode (day surgery or non-day surgery), operation duration (min), surgical approach, operative segment, smoking and drinking status, diabetes, hypertension, occupational lifting, sedentary occupation, the amount of active straight-leg raise exercises after first surgery (lack of active straight-leg raise exercises was defined as less than 20 active straight-leg raise exercises per day on average within 1 month after the operation). The preoperative imaging data included disc height index (DHI) (Figure 1), endplate concave angle (ECA) (Figure 2), segmental range of motion (SROM) (Figure 3), lumbar lordosis (LL), sacral slope (SS), the grade of disc degeneration (Pfirrmann classification) [10], herniated disc location, and Modic changes (MCs) [11]. Measures of DHI, sROM, ECA, grade of disc degeneration, herniated disc location, and MCs were performed in the surgical segment. The data were gathered and examined by an experienced spine surgeon who was not involved in the surgical procedure. In addition, recurrence of LDH (rLDH) was defined as relapse of LDH at the same level and on the same side, and the painless interval was at least 1 month after surgery [12]. Incomplete removal of the herniated disc was defined as the herniated disc still compressed the nerve root as confirmed by postoperative imaging, and the symptoms of nerve root compression were persistent presence after PELD [13].
STATISTICAL ANALYSIS:
All statistical analyses were performed using SPSS (version 25.0; IBM, USA). Categorical variables were expressed as counts and percentages, and continuous variables were presented in the form of mean±standard deviation (SD). A matched case-control design was used to determine the associated risk factors for reoperation. The case group was composed of patients with reoperation, while the control group was composed of patients without reoperation. The case group and control group were matched according to the date of surgery, and the matching ratio was 1: 3. Univariate analysis was performed using the independent samples
Results
PATIENT’S DEMOGRAPHIC AND CLINICAL CHARACTERISTICS:
A total of 435 patients who underwent single-level PELD with at least 2 years of follow-up time were included in this study. The follow-up time ranged from 24 to 58 months (34.8±13.8 months). We determined the cause of reoperation based on the patient’s postoperative physical examination, clinical situation, laboratory tests, and imaging examinations. The reoperation rate of all patients during the follow-up period was 6.2% (27/435) (Table 1). Among all patients, 27 (15 men and 12 women, with an average age of 57.6±14.1 years, range, 21–81) underwent reoperation. A total of 81 patients were selected as matched controls from the remaining 408 patients without reoperation. The causes and rates of reoperation are as follows: recurrence of LDH, 3.2% (14/435); incomplete decompression, 1.8% (8/435); persistent low back pain, 0.7% (3/435); and postoperative infection, 0.5% (2/435). Among the 27 patients who underwent reoperation, 10 were treated with PELD, 10 were treated with posterior lumbar fusion, 3 were treated with lumbar radiofrequency thermocoagulation, and 2 were treated with spinal endoscopic removal of the infected lesion.
Univariate analysis was performed for the clinical parameters and radiological parameters (Table 2). There were 27 patients in the case group and 81 in the control group. Of these factors, age (P=0.015), Pfirrmann grade IV–V (P=0.017), and lack of active straight-leg raise exercises postoperatively (P=0.026) were significantly related to the reoperation after PELD. Based on this univariate analysis, we performed multiple logistic regression analysis, which showed that age (P=0.001), Pfirrmann grade IV–V (P=0.033), and lack of active straight-leg raise exercises postoperatively (P=0.003) were independent risk factors for reoperation after PELD (Table 3).
CASE 1: A 65-year-old woman had severe pain on the lateral side of her right leg for nearly 3 months. Her axial T2-weighted MRI showed a herniated disc on the right side at level L5-S1, then she underwent right L5-S1 PELD in our hospital. Pain in the right leg was significantly relieved after surgery, and she discharged from the hospital the day after PELD. However, 3 years later, she again had continuous radiating pain in the right leg, with severe low back pain and restriction of low back motion. MRI reexamination found a herniated disc on the right side at level L5-S1 with severe foraminal stenosis. She was diagnosed with L5-S1 rLDH. Because she had no obvious improvement after 1 month of conservative treatment, combined with clinical symptoms and imaging examination of the patient, L5-S1 minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) was performed by the same surgeon. The radiating pain in the right leg and severe low back pain were obviously relieved after reoperation, and there was no recurrence of right leg pain during the subsequent follow-up period (Figure 4).
CASE 2: A 57-year-old man had severe radiating right leg pain for 6 months. His axial T2-weighted MR image showed a herniated disc on the right side at level L4–5. He received a PELD with transforaminal approach in our hospital, but his right leg pain was not relieved. MRI reexamination still indicated a herniated disc on the right side at level L4–5 at 1 month after PELD, likely due to incomplete removal of the herniated disc. Therefore, PELD at the same level of was performed again by the same surgeon via interlaminar approach 2 months later, and the pain in the right leg disappeared after reoperation (Figure 5).
Discussion
REASONS FOR REOPERATION:
Our study showed that recurrence LDH was a common cause of reoperation after PELD in 435 patients with at least 2 years of follow-up. In this study, the rate of reoperation caused by rLDH was 3.2%, which is lower than the 7.0–17.6% recurrence rate reported in the literature [18–20], perhaps because all patients were operated on by surgeons with sufficient experience in PELD. Incomplete decompression is also a common reason for reoperation after PELD. The location, type, and size of the disc herniation are closely associated with incomplete decompression [5]. In general, surgeons still use the transforaminal approach of PELD for most patients with L4/5 central-type or paramedian-type LDH; however, due to the limitation of anatomical structure, in some patients it is difficult to directly remove the herniated disc (Figure 5). Therefore, the symptoms of nerve root compression are not relieved effectively after PELD, so the decompression surgery has to be performed again. Beyond that, in the cases of our study, 2 patients had postoperative infection, and spinal endoscopic removal of the infected lesion was performed. There were also 2 patients who underwent lumbar radiofrequency thermocoagulation due to persistent low back pain after PELD, and the low back pain was effectively relieved after the operation.
RISK FACTORS FOR REOPERATION:
Many previous studies have focused on the related complications after PELD [21,22]. However, few studies have reported the risk factors for reoperation after PELD. In this study, we investigated the basic characteristics and the imaging parameters of patients, using a matched case-control design and univariate analysis to determine the clinical and radiological risk factors leading to reoperation. The present study found that age, active straight-leg raise exercises, and grade of disc degeneration were significantly associated with reoperation after PELD, indicating that spine surgeons should careful and gently perform the operation when treating these patients.
AGE AND PFIRRMANN GRADE ARE CLOSELY RELATED TO REOPERATION:
Previous studies have shown that the reoperation rate of elderly patients after lumbar surgery is significantly higher, which is consistent with our conclusions [6]. We believe that patients older patients tend to have more serious degeneration of intervertebral discs and lumbar facet joints. Hwang et al [23] found that intervertebral disc degeneration (Pfirrmann IV) is a risk factor for disc herniation or foraminal stenosis requiring reoperation after microdecompression in patients with lumbar spinal stenosis. For patients with severe intervertebral disc degeneration and lumbar facet joint degeneration, the height of the intervertebral space tends to be significantly less, with and plenty of osteophyte hyperplasia in the lumbar facet joint, so it is difficult to select the appropriate channel position, the operation field of vision is worse, and the operation space is smaller during PELD, which increases the difficulty of the operation. The reduced intervertebral space height leads to narrowing of the intervertebral foramen and causes compression of the nerve roots. In addition, due to severe degeneration of intervertebral discs in elderly patients, the ability of self-repair is worse. These conditions lead to a higher reoperation rate in older patients with severe lumbar disc degeneration.
ACTIVE STRAIGHT-LEG RAISE EXERCISES IS CLOSELY RELATED TO REOPERATION:
Active straight-leg raise exercise is also significantly related to reoperation. Kara et al [24] showed that lack of physical exercise is a significant predictor of reoperation after lumbar discectomy. Our results revealed that among the patients who received reoperation, 66.7% (18/27) did not perform active straight-leg raise exercises after PELD. We believe that in the process of active straight-leg raise exercises, the nerve roots can be properly pulled to help reduce the adhesion of nerve roots after surgery, and it can also promote rehabilitation of lower-limb muscle strength. In addition, we recommend that patients stay in bed as much as possible for 1 month to reduce nerve root edema and promote healing of the annulus fibrosus. For all patients after PELD, we explain the situation and encourage them to perform active straight-leg raise exercises before discharge, but most patients did not due to poor medical compliance. Therefore, we have included this factor in this study, and the results confirm our preliminary idea that patients who do not perform active straight-leg raise exercises are more likely to undergo reoperation.
LIMITATIONS:
This study has some limitations. First, this was a single-center, retrospective study, and there were relatively few patients in the case group, so there may have been selection bias. The outcomes of the current study must be confirmed in a prospective trial with a larger patient sample. Second, the follow-up time was relatively short, which could also have affected the rate of reoperation.
Conclusions
PELD is an effective and minimally invasive method to treat LDH. In our study, the reoperation rate of PELD was 6.2%. The main reason for reoperation was recurrence of LDH. In addition, we also found that severe disc degeneration, older age, and lack of active straight-leg raise exercises significantly increased the rate of reoperation.
Figures
![Measurement of the DHI: The height of the anterior a), middle b), and posterior c) intervertebral space and the sagittal diameter of the overlying vertebral body d) were measured. DHI=[(a+b+c)/3]/d.](https://jours.isi-science.com/imageXml.php?i=medscimonit-29-e939844-g001.jpg&idArt=939844&w=1000) Figure 1. Measurement of the DHI: The height of the anterior a), middle b), and posterior c) intervertebral space and the sagittal diameter of the overlying vertebral body d) were measured. DHI=[(a+b+c)/3]/d.
Figure 1. Measurement of the DHI: The height of the anterior a), middle b), and posterior c) intervertebral space and the sagittal diameter of the overlying vertebral body d) were measured. DHI=[(a+b+c)/3]/d. 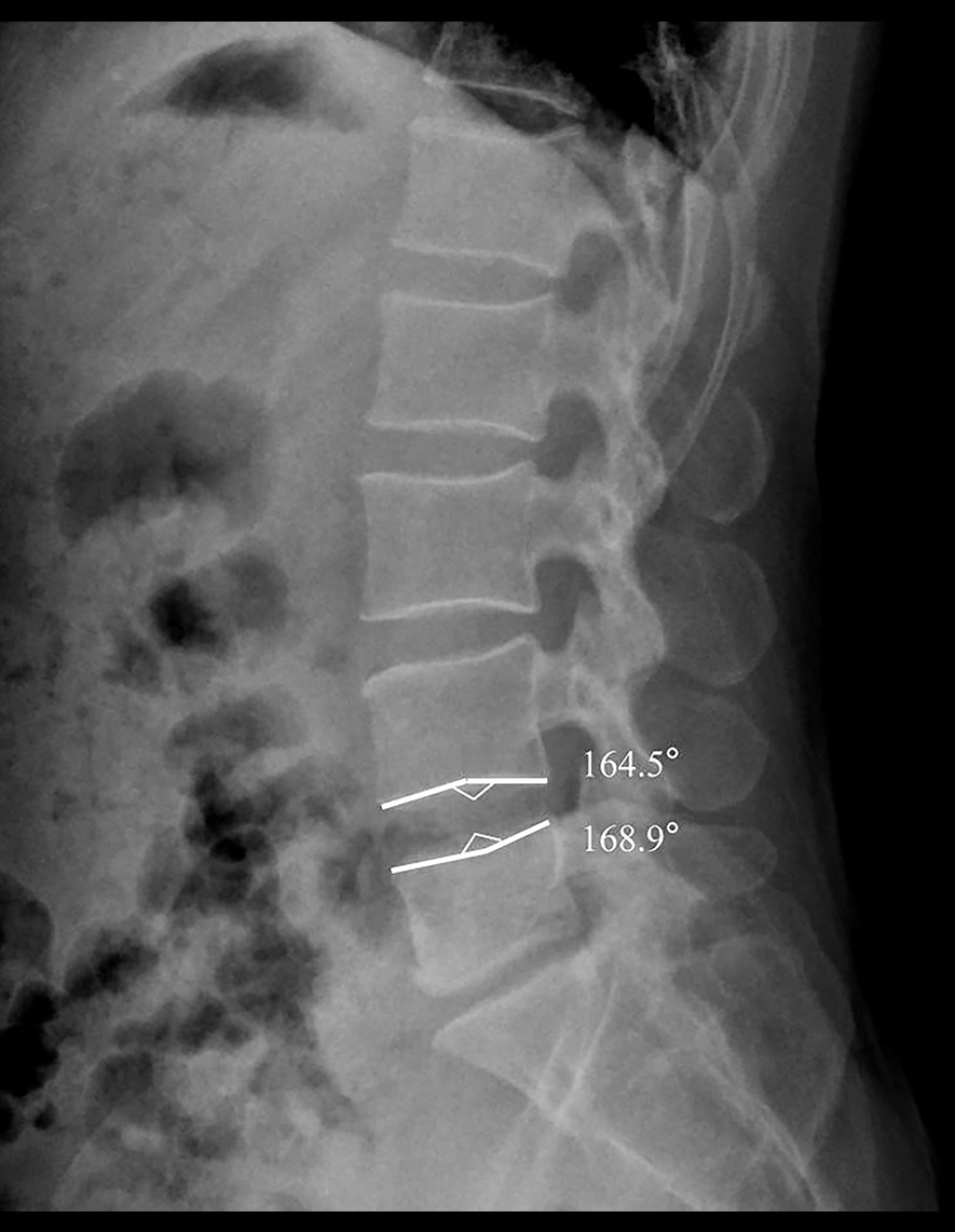 Figure 2. Measurement of the ECA: On the sagittal X-ray of the lumbar spine, the bone endplate of lumbar vertebra is in arc shape, and a line was drawn from the summit/bottom of arc along to the endpoints, and the angle between these 2 lines is defined as the ECA.
Figure 2. Measurement of the ECA: On the sagittal X-ray of the lumbar spine, the bone endplate of lumbar vertebra is in arc shape, and a line was drawn from the summit/bottom of arc along to the endpoints, and the angle between these 2 lines is defined as the ECA.  Figure 3. Measurement of the sROM: (A, B) The sROM can be calculated by the difference between flexion and extension angles, which was measured in relation to the lines of the superior and inferior endplate of the surgical level. The patient sROM is 9.8 degrees at L4–L5 in this patient.
Figure 3. Measurement of the sROM: (A, B) The sROM can be calculated by the difference between flexion and extension angles, which was measured in relation to the lines of the superior and inferior endplate of the surgical level. The patient sROM is 9.8 degrees at L4–L5 in this patient. 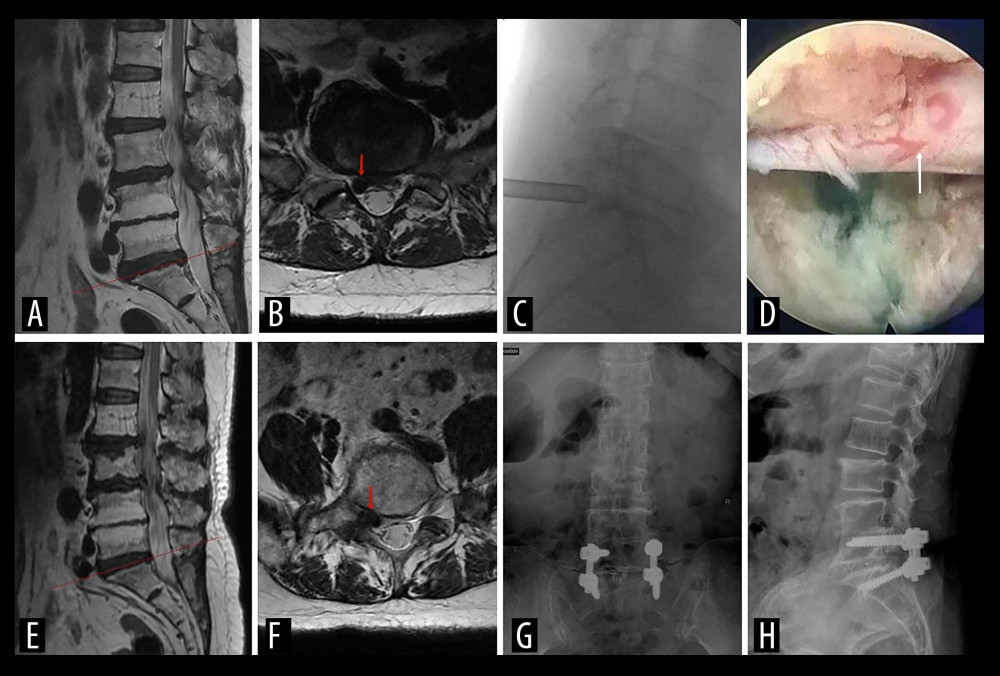 Figure 4. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L5-S1 (red arrow). (C) The working channels of interlaminar approach. (D) The decompressed nerve root under endoscopic view (white arrow). (F, F) Three years later, MRI reexamination showed the herniated disc on the right side at level L5-S1 with severely foraminal stenosis (red arrow). (G, H) X-ray examination of lumbar vertebrae after reoperation.
Figure 4. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L5-S1 (red arrow). (C) The working channels of interlaminar approach. (D) The decompressed nerve root under endoscopic view (white arrow). (F, F) Three years later, MRI reexamination showed the herniated disc on the right side at level L5-S1 with severely foraminal stenosis (red arrow). (G, H) X-ray examination of lumbar vertebrae after reoperation. 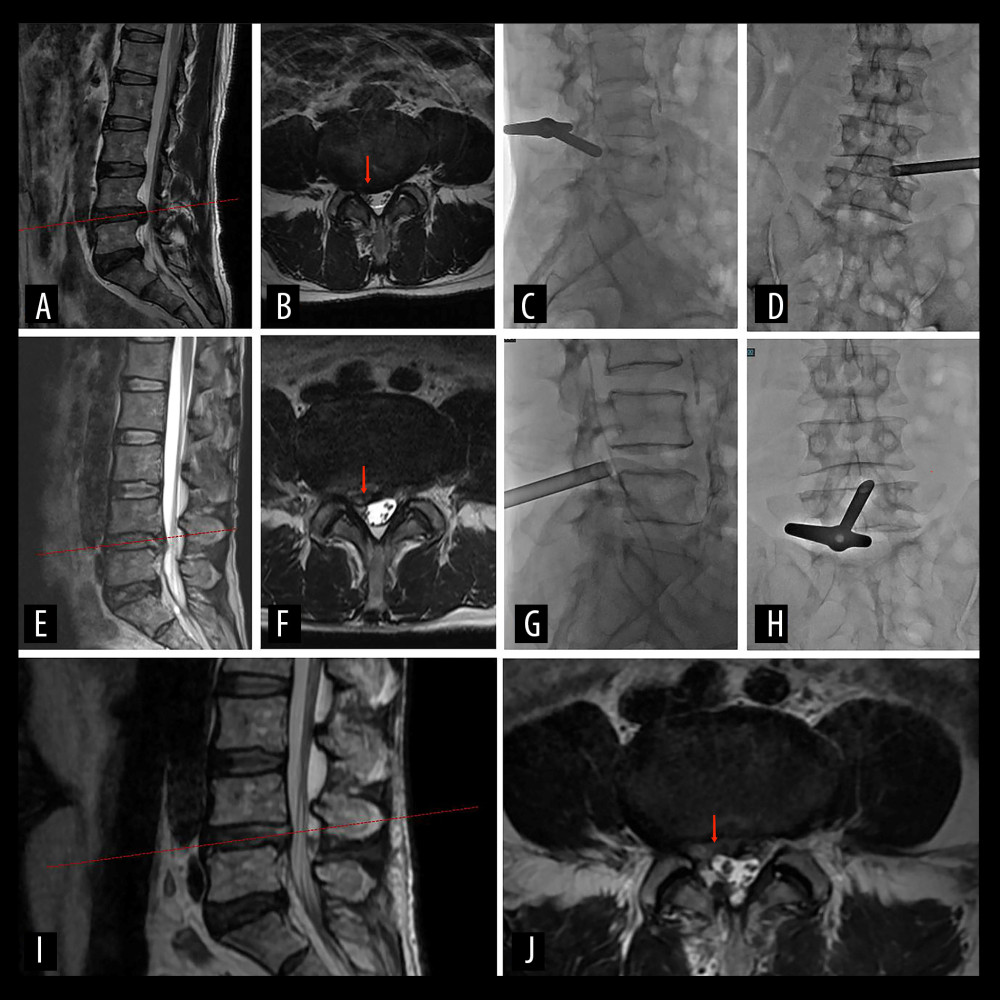 Figure 5. A 57-year-old man with severe right leg radiating pain for 6 months. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L4–L5 (red arrow). (C, D) The working channels of transforaminal approach during the first PELD. (E, F) MRI reexamination at 1 month after the first PELD. The red arrow indicates residual intervertebral disc tissue. (G, H) The working channels of interlaminar approach. (I, J) MRI reexamination showed the dural sac was well-filled and there was no compression of nerve roots after reoperation (red arrow).
Figure 5. A 57-year-old man with severe right leg radiating pain for 6 months. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L4–L5 (red arrow). (C, D) The working channels of transforaminal approach during the first PELD. (E, F) MRI reexamination at 1 month after the first PELD. The red arrow indicates residual intervertebral disc tissue. (G, H) The working channels of interlaminar approach. (I, J) MRI reexamination showed the dural sac was well-filled and there was no compression of nerve roots after reoperation (red arrow). References
1. Li L, Chang F, Hai Y, Clinical effect evaluation and correlation between preoperative imaging parameters and clinical effect of endoscopic transforaminal decompression for lumbar spinal stenosis: BMC Musculoskelet Disord, 2020; 21(1); 68
2. Cao J, Huang W, Wu T, Percutaneous endoscopic lumbar discectomy for lumbar disc herniation as day surgery: Short-term clinical results of 235 consecutive cases: Medicine (Baltimore), 2019; 98(49); e18064
3. Kambin P, Sampson S, Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results: Clin Orthop Relat Res, 1986(207); 37-43
4. Gadjradj PS, Harhangi BS, Full-endoscopic transforaminal discectomy versus open microdiscectomy for sciatica: Update of a systematic review and meta-analysis: Spine (Phila Pa 1976), 2022; 47(18); E591-E94
5. Choi KC, Lee JH, Kim JS, Unsuccessful percutaneous endoscopic lumbar discectomy: A single-center experience of 10,228 cases: Neurosurgery, 2015; 76(4); 372-81
6. Wang H, Zhou Y, Li C, Risk factors for failure of single-level percutaneous endoscopic lumbar discectomy: J Neurosurg Spine, 2015; 23(3); 320-25
7. Pan M, Li Q, Li S, Percutaneous endoscopic lumbar discectomy: Indications and complications: Pain Physician, 2020; 23(1); 49-56
8. Ruan W, Feng F, Liu Z, Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: A meta-analysis: Int J Surg, 2016; 31; 86-92
9. Aihara T, Endo K, Sawaji Y, Five-year reoperation rates and causes for reoperations following lumbar microendoscopic discectomy and decompression: Spine (Phila Pa 1976), 2020; 45(1); 71-77
10. Pfirrmann CW, Metzdorf A, Zanetti M, Magnetic resonance classification of lumbar intervertebral disc degeneration: Spine (Phila Pa 1976), 2001; 26(17); 1873-78
11. Modic MT, Steinberg PM, Ross JS, Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging: Radiology, 1988; 166(1 Pt 1); 193-99
12. Shi H, Zhu L, Jiang ZL, Radiological risk factors for recurrent lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: A retrospective matched case-control study: Eur Spine J, 2021; 30(4); 886-92
13. Gadjradj PS, Rubinstein SM, Peul WC, Full endoscopic versus open discectomy for sciatica: Randomised controlled non-inferiority trial: BMJ, 2022; 376; e065846
14. Gadjradj PS, Broulikova HM, van Dongen JM, Cost-effectiveness of full endoscopic versus open discectomy for sciatica: Br J Sports Med, 2022; 56(18); 1018-25
15. Lang Z, Li JS, Yang F, Reoperation of decompression alone or decompression plus fusion surgeries for degenerative lumbar diseases: A systematic review: Eur Spine J, 2019; 28(6); 1371-85
16. Häkkinen A, Kiviranta I, Neva MH, Reoperations after first lumbar disc herniation surgery; A special interest on residives during a 5-year follow-up: BMC Musculoskelet Disord, 2007; 8; 2
17. Kong M, Xu D, Gao C, Risk factors for recurrent L4–5 disc herniation after percutaneous endoscopic transforaminal discectomy: A retrospective analysis of 654 cases: Risk Manag Healthc Policy, 2020; 13; 3051-65
18. Yu C, Zhan X, Liu C, Risk factors for recurrent L5-S1 disc herniation after percutaneous endoscopic transforaminal discectomy: A retrospective study: Med Sci Monit, 2020; 26; e919888
19. Shin EH, Cho KJ, Kim YT, Risk factors for recurrent lumbar disc herniation after discectomy: Int Orthop, 2019; 43(4); 963-67
20. Fan N, Yuan S, Du P, Complications and risk factors of percutaneous endoscopic transforaminal discectomy in the treatment of lumbar spinal stenosis: BMC Musculoskelet Disord, 2021; 22(1); 1041
21. Zhou C, Zhang G, Panchal RR, Unique complications of percutaneous endoscopic lumbar discectomy and percutaneous endoscopic interlaminar discectomy: Pain Physician, 2018; 21(2); E105-E12
22. Hwang HJ, Park HK, Lee GS, Predictors of reoperation after microdecompression in lumbar spinal stenosis: Korean J Spine, 2016; 13(4); 183-89
23. Kara B, Tulum Z, Acar U, Functional results and the risk factors of reoperations after lumbar disc surgery: Eur Spine J, 2005; 14(1); 43-48
Figures
 Figure 1. Measurement of the DHI: The height of the anterior a), middle b), and posterior c) intervertebral space and the sagittal diameter of the overlying vertebral body d) were measured. DHI=[(a+b+c)/3]/d.
Figure 1. Measurement of the DHI: The height of the anterior a), middle b), and posterior c) intervertebral space and the sagittal diameter of the overlying vertebral body d) were measured. DHI=[(a+b+c)/3]/d.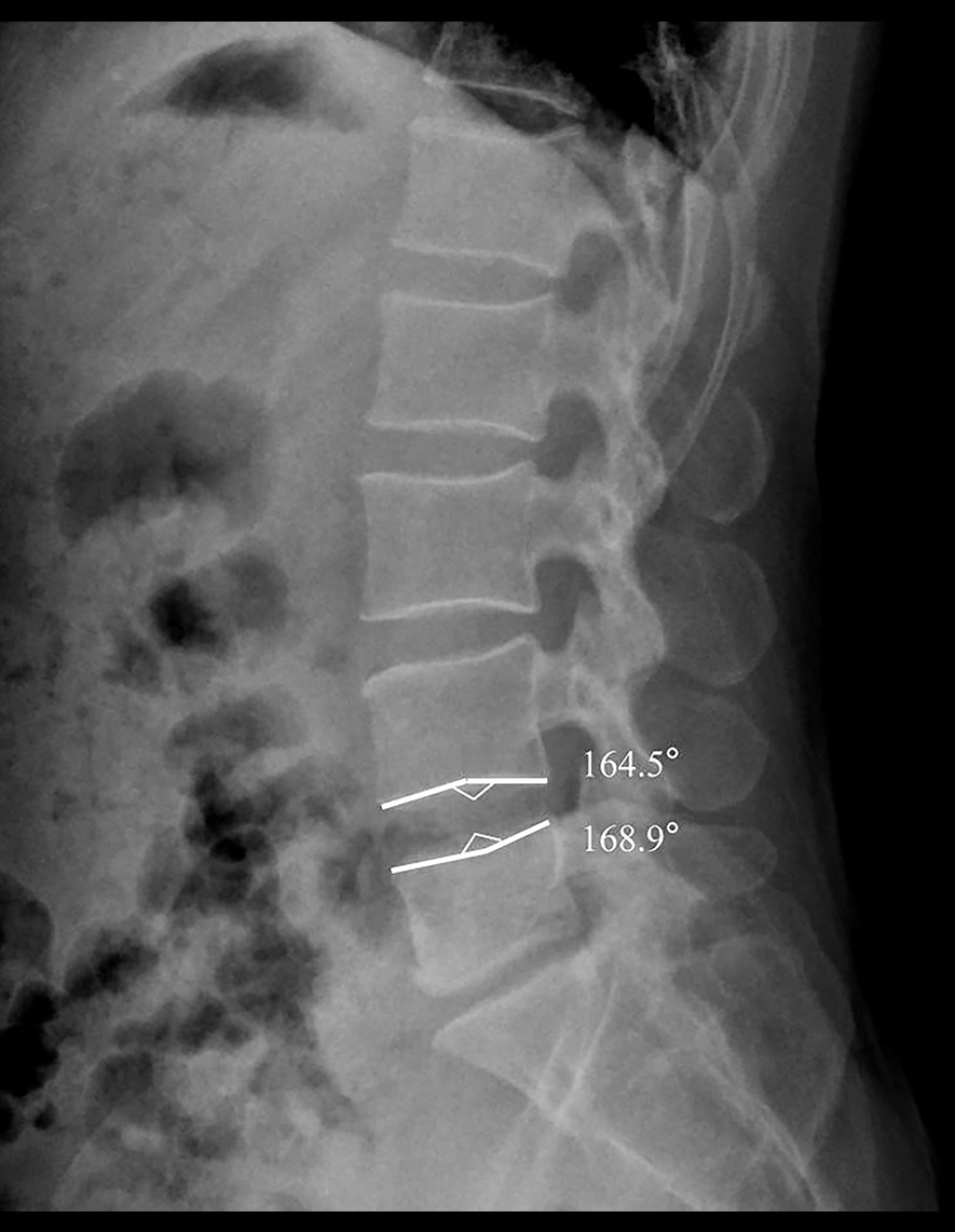 Figure 2. Measurement of the ECA: On the sagittal X-ray of the lumbar spine, the bone endplate of lumbar vertebra is in arc shape, and a line was drawn from the summit/bottom of arc along to the endpoints, and the angle between these 2 lines is defined as the ECA.
Figure 2. Measurement of the ECA: On the sagittal X-ray of the lumbar spine, the bone endplate of lumbar vertebra is in arc shape, and a line was drawn from the summit/bottom of arc along to the endpoints, and the angle between these 2 lines is defined as the ECA. Figure 3. Measurement of the sROM: (A, B) The sROM can be calculated by the difference between flexion and extension angles, which was measured in relation to the lines of the superior and inferior endplate of the surgical level. The patient sROM is 9.8 degrees at L4–L5 in this patient.
Figure 3. Measurement of the sROM: (A, B) The sROM can be calculated by the difference between flexion and extension angles, which was measured in relation to the lines of the superior and inferior endplate of the surgical level. The patient sROM is 9.8 degrees at L4–L5 in this patient.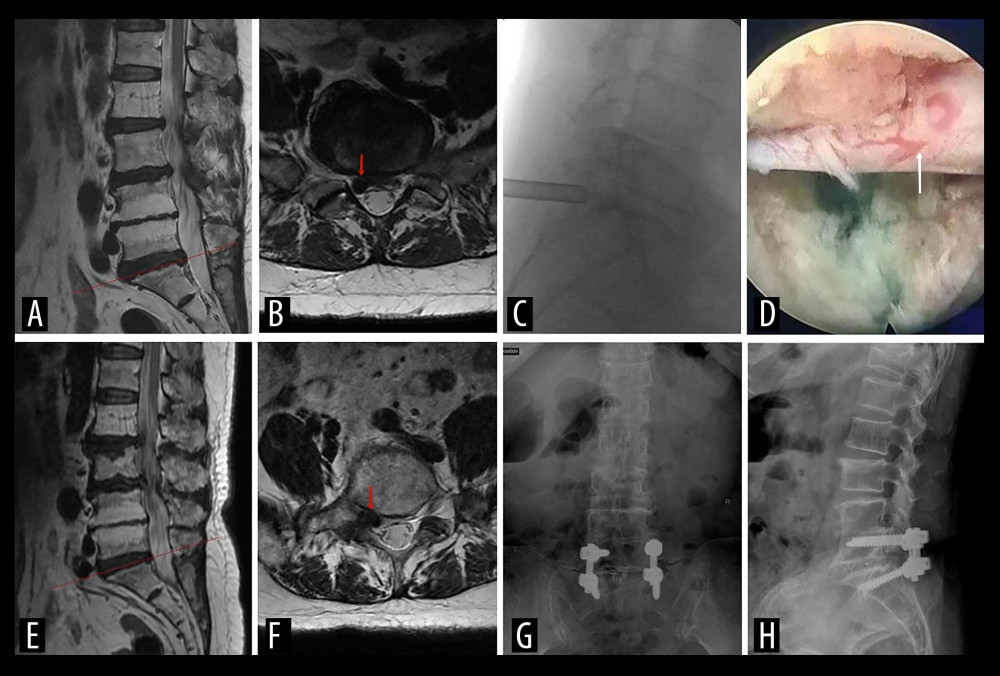 Figure 4. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L5-S1 (red arrow). (C) The working channels of interlaminar approach. (D) The decompressed nerve root under endoscopic view (white arrow). (F, F) Three years later, MRI reexamination showed the herniated disc on the right side at level L5-S1 with severely foraminal stenosis (red arrow). (G, H) X-ray examination of lumbar vertebrae after reoperation.
Figure 4. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L5-S1 (red arrow). (C) The working channels of interlaminar approach. (D) The decompressed nerve root under endoscopic view (white arrow). (F, F) Three years later, MRI reexamination showed the herniated disc on the right side at level L5-S1 with severely foraminal stenosis (red arrow). (G, H) X-ray examination of lumbar vertebrae after reoperation.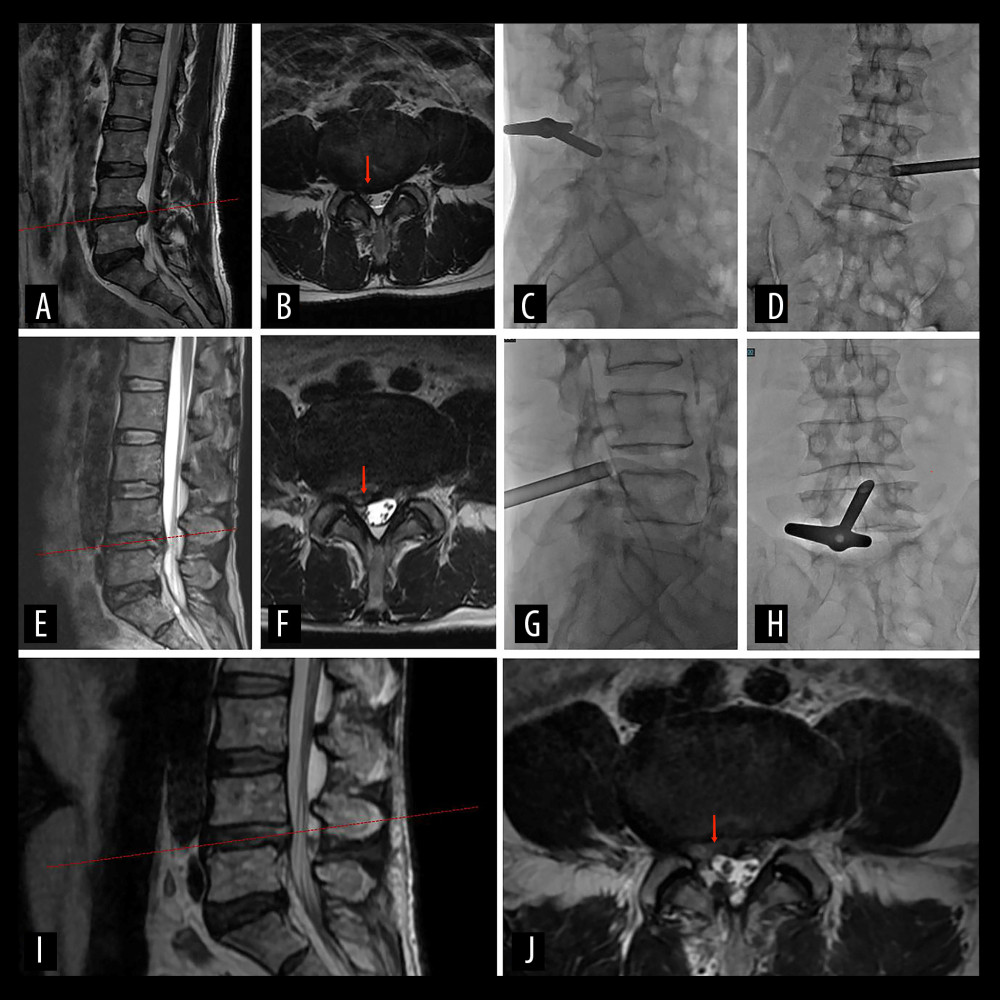 Figure 5. A 57-year-old man with severe right leg radiating pain for 6 months. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L4–L5 (red arrow). (C, D) The working channels of transforaminal approach during the first PELD. (E, F) MRI reexamination at 1 month after the first PELD. The red arrow indicates residual intervertebral disc tissue. (G, H) The working channels of interlaminar approach. (I, J) MRI reexamination showed the dural sac was well-filled and there was no compression of nerve roots after reoperation (red arrow).
Figure 5. A 57-year-old man with severe right leg radiating pain for 6 months. (A, B) Preoperative MRI scan shows the segment of lumbar disc herniation at L4–L5 (red arrow). (C, D) The working channels of transforaminal approach during the first PELD. (E, F) MRI reexamination at 1 month after the first PELD. The red arrow indicates residual intervertebral disc tissue. (G, H) The working channels of interlaminar approach. (I, J) MRI reexamination showed the dural sac was well-filled and there was no compression of nerve roots after reoperation (red arrow). Tables
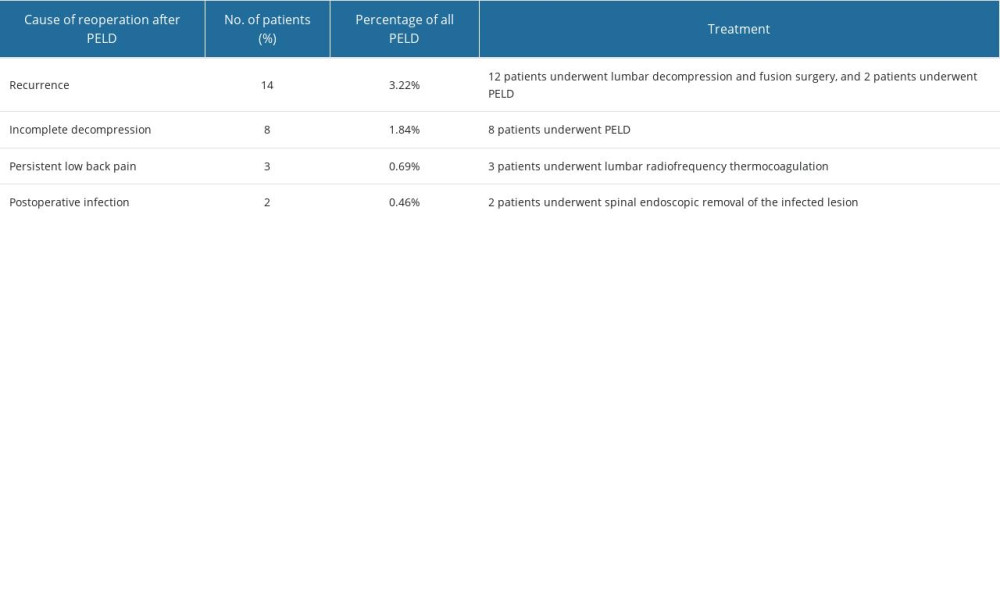 Table 1. Cause of reoperation after PELD.
Table 1. Cause of reoperation after PELD.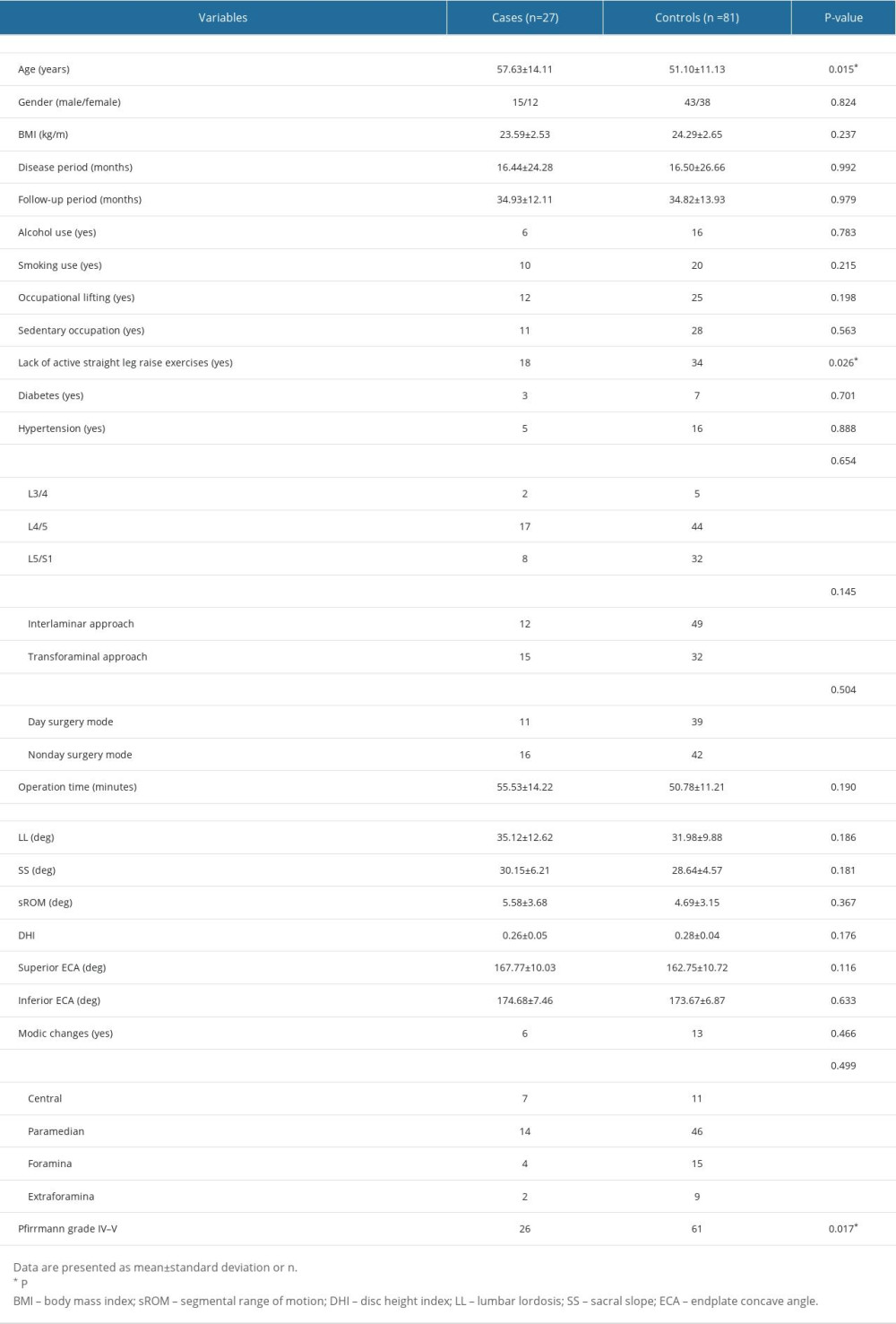 Table 2. Univariate analyses of clinical characteristics and preoperative radiological findings.
Table 2. Univariate analyses of clinical characteristics and preoperative radiological findings.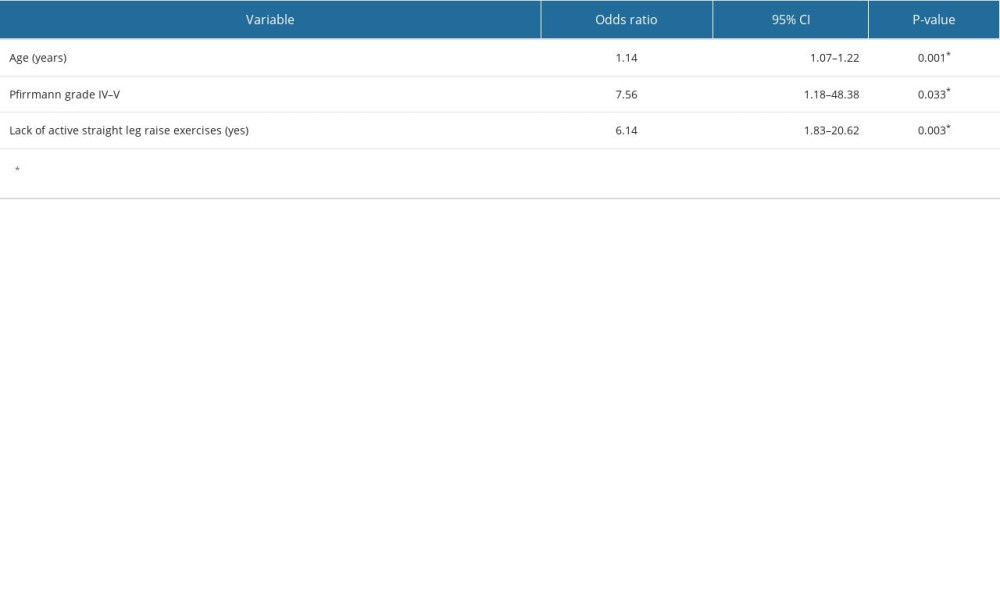 Table 3. Multiple logistic regression analysis: independent risk factors of reoperation.
Table 3. Multiple logistic regression analysis: independent risk factors of reoperation.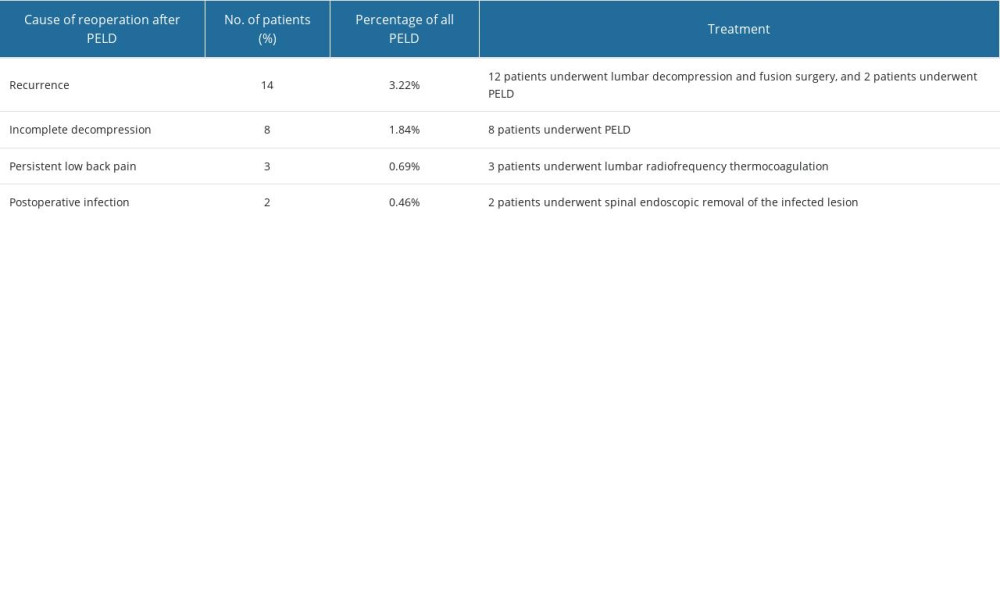 Table 1. Cause of reoperation after PELD.
Table 1. Cause of reoperation after PELD.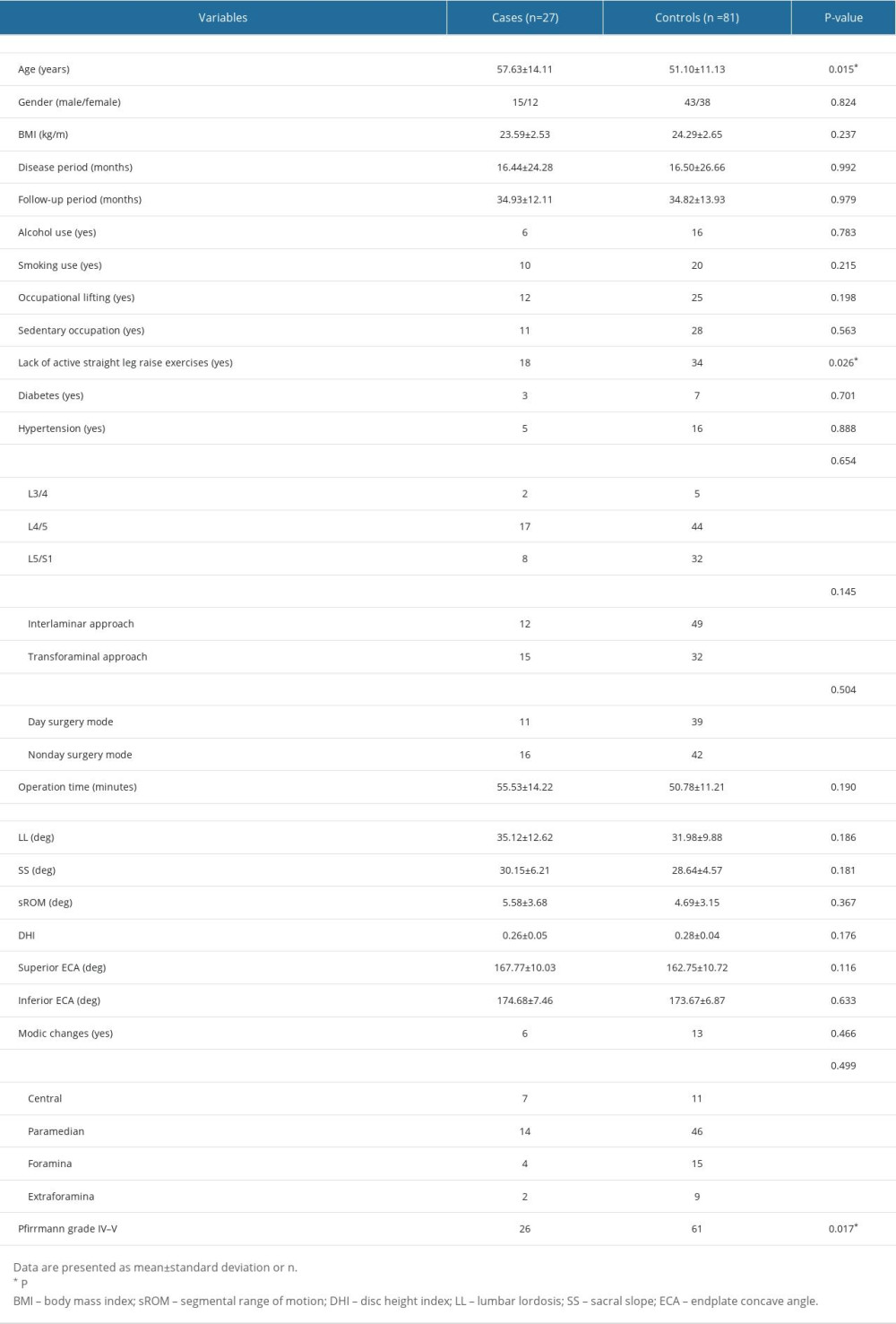 Table 2. Univariate analyses of clinical characteristics and preoperative radiological findings.
Table 2. Univariate analyses of clinical characteristics and preoperative radiological findings.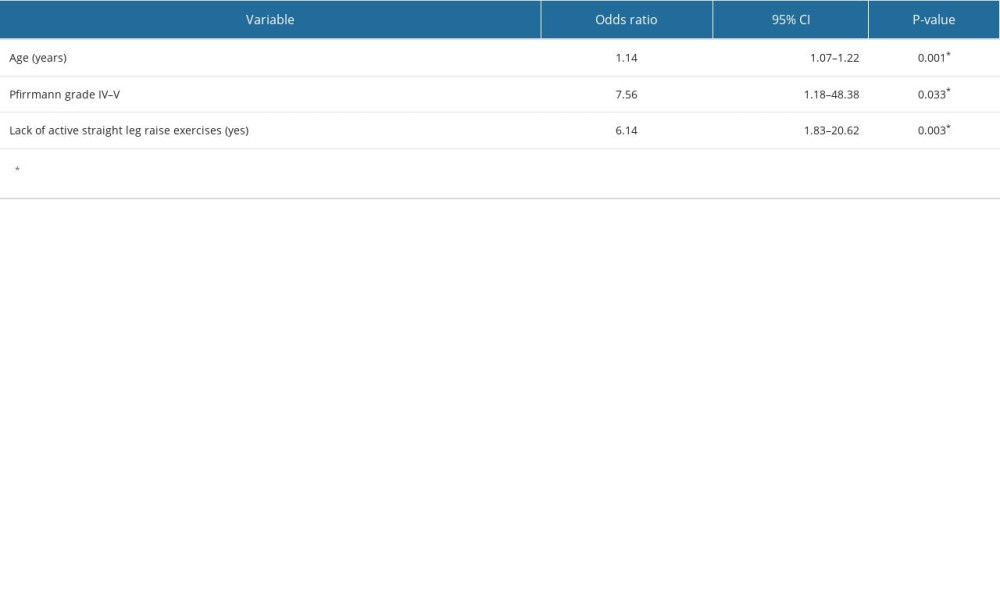 Table 3. Multiple logistic regression analysis: independent risk factors of reoperation.
Table 3. Multiple logistic regression analysis: independent risk factors of reoperation. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








