07 September 2023: Clinical Research
Comparative Biomechanical Analysis of Anterior Process Locking Plate Alone versus Combined with Percutaneous Cannulated Screw Fixation for Sanders Type II Calcaneal Fractures: A Finite Element Study
Rongji Ma1ABCEF, Atik Badshah Shaikh2BCDEF, Qinxin Zhang1ABCEF, Xiuyun Su2CDE, Yonghua Wang1BC, Fuhai Pan2BC, Jianwen Chen2ACDEG, Kai He2ABCDEG*DOI: 10.12659/MSM.940300
Med Sci Monit 2023; 29:e940300
Abstract
BACKGROUND: Calcaneal fractures are the most common tarsal bone fractures, and account for 75% of intra-articular fractures. The purpose of this study was to compare the biomechanical stability of the anterior process locking plate combined with the percutaneous cannulated screw fixation (screw group) versus the anterior process locking plate fixation alone (plate group) for the treatment of Sanders type II calcaneal fractures using finite element analysis to provide a theoretical basis for clinical work.
MATERIAL AND METHODS: We established a 3D model of Sanders type II calcaneal fracture; assigned material properties to the internal fixation systems; applied loads; set up analysis criteria; analyzed the displacement of the fracture, relative displacement, stress state of bone tissue, and internal fixation; and compared mechanical stability.
RESULTS: For Sanders type II A, II B, and II C calcaneal fractures, the degree of displacement and relative displacement of the fracture in the screw group was less than that of the plate group. For all subtypes of Sanders type II calcaneal fractures, the screw group had better mechanical stability than the plate group.
CONCLUSIONS: Both fixation methods (screw and plate group) were within a reasonable range for restoring the levelling effect of the joint surface and maintaining the strength of fixation, and both had good mechanical stability. Finite element analysis is a relatively reliable method, and biomechanics and clinical studies must further verify the experimental results.
Keywords: Fracture Fixation, Internal, Finite Element Analysis, Biomechanical Phenomena, Calcaneus, Humans, Fractures, Bone, intra-articular fractures, Ankle Injuries, Bone Screws, Knee Injuries
Background
Calcaneal fractures are the most common tarsal bone fractures, accounting for 60% of all tarsal fractures, and among the calcaneal fractures, 75% are intra-articular calcaneal fractures [1,2]. Conservative treatment of these fractures often produces unsatisfactory functional outcomes, such as malunion and subtalar joint arthritis [3]. Surgical treatment by open reduction and internal fixation (ORIF) with plates and screws is still the standard treatment. However, it also has a high rate of postoperative complications, including deep infection and cutaneous nerve injury [4]. Hence, an appropriate surgical approach combined with fixation stability is critical to achieving a suitable outcome for calcaneal fractures. Several minimally invasive osteosynthesis techniques have recently been used to treat intra-articular calcaneal fractures [5].
Sanders classification is the most commonly used classification system for calcaneal fractures; it relies on computed tomography (CT)-generated images to describe the location and number of fracture lines through the posterior facet. Sanders classification has a vital clinical role in selecting treatment methods and prognosis of calcaneal fractures. Sanders II type calcaneal fractures treatment with ORIF via an extended lateral approach is becoming popular, as it provides adequate exposure and restores anatomical alignment of the calcaneum and congruity of the posterior subtalar joint, and produces stable fixation [6]. However, this approach has a high risk of deep and superficial infection, wound edge necrosis, and nerve damage [7]. In recent years, the sinus tarsi approach (STA), a minimally invasive reduction and fixation technique, has been widely used in the clinical setting to overcome potential complications from an extended lateral approach [8,9].
Using the invasive sinus tarsi approach, anterior process locking plate fixation combined with percutaneous cannulated screws fixation or a simple anterior process locking plate fixation alone is used to fix the calcaneal fracture. The locking plates provide sufficient stability and support in the coronal plane and the medial segment of the calcaneus; moreover, the locking plates cannot always engage all the fracture fragments and usually require additional percutaneous cannulated screws fixation. Over the years, several biomechanical studies have focused on calcaneal fractures based on various models [10,11]. Finite element analysis (FEA) models overcome the need for cadaveric studies and provide a unique platform to evaluate internal strain and stress on the bone and implants. It has been commonly used to assess the biomechanics and stability of individual implants and to understand the mechanism of adverse trauma events [12–15]. Moreover, FEA has been used to analyze the internal pressure distribution of the foot in disorders such as flatfoot, clubfoot, and Lisfranc joint injuries [16].
However, the mechanical stability provided by a locking plate combined with percutaneous screws fixation or a simple locking plate fixation alone is still controversial and must be verified. Therefore, basic research on the biomechanical stability of the internal fixation system for Sanders II type calcaneal fractures is fundamentally warranted. This study compared the biomechanical stability of anterior process locking plate combined with percutaneous cannulated screws fixation (screw group) with traditional anterior process locking plate fixation alone (plate group) in treating Sanders type II calcaneal fractures using FEA.
Material and Methods
PARTICIPANT AND CT SCANNING:
The right foot of a male volunteer underwent a CT scan in a neutral, non-weight-bearing position (Siemens SOMATOM Force dual-source CT). The male volunteer was 26 years old (he provided signed informed consent), height 177 cm, and body weight 75 kg, without deformity, and had no history of foot trauma, foot and ankle diseases, osteoarthritis, or cancer. The hospital’s Ethics Committee approved the study. The scanning length was 25 cm above the ankle to the planta pedis. Imaging parameters of the CT scan were: scan thickness 0.625 mm, 155 mAs at tube voltage 120 kV, matrix, 512×512. A total of 1019 images were obtained from the CT scan and were saved in DICOM 3.0 format.
GEOMETRICAL RECONSTRUCTION:
To obtain a 3D model of the calcaneus bone, the CT scan data (DICOM format) were transferred to Mimics 13.0 software (Materialise NV, Leuven, Belgium) to obtain a computer-aided design (CAD) model. All bony components of the foot and ankle were distinguished by 3D interactive and automatic segmentation. The model underwent wrapping, denoising, smoothing, and surface fitting using Geomagic Design X software (Geomagic, Inc, Research Triangle Park, NC, USA) to obtain a geometric calcaneus model of 94 135 elements and 25 048 nodes.
Sanders type II calcaneal fracture models were built by importing 3D calcaneus models to the SolidWorks 2021 software (Dassault Systemes, SolidWorks Corporation, MA, USA) and using the cutting tools to establish 3 types of calcaneal fractures (A, B, C) (Figure 1). For Sanders type II A, a single primary fracture line courses through the lateral aspect of the poster facet; for Sanders type II B, a single primary fracture line courses through the central aspect of the posterior facet; and for Sanders type II C, a single primary fracture line courses through the medial aspect of the posterior facet. Different fracture fragments were designed as a complete fracture plane model, and the friction coefficient was set to 0.2.
To create 3D models of the plate and screws, a Tianyuan 3D scanner and retrograde engineering scanner were used to scan the anterior process locking plate, screws, and 5.2-mm percutaneous cannulated screws (Ideal Medical Instrument Company, Jiangsu, China). The anterior process locking plate was positioned and aligned by an experienced orthopedic surgeon according to the manufacturer’s instructions and the surgeon’s clinical experience. On each model of Sanders type II (A, B, C) calcaneal fracture, the anterior process locking plate was placed on the lateral side of the calcaneus and fixation screws were inserted to avoid displacement of plates to the other side of the cortical bone or an articular surface. In contrast, the two 5.2-mm percutaneous cannulated screws were driven from the calcaneal tuberosity toward the calcaneocuboid joint or posterior facet (Figure 2) to bridge the anterior and posterior fragments. Six groups of models were established and finally imported into ANSYS 13.0 software for finite element analysis.
MATERIAL PROPERTIES, BOUNDARY CONDITIONS, AND LOADING CRITERIA:
For materials properties of the finite element model, titanium plates and screws were assigned according to previous reports in the literature [17] and simplified to be homogeneous and isotropic. The material properties are listed in Table 1.
Assuming the fracture lines are complete and there is possible contact between fracture segments after loading, the friction coefficient of 0.2 was assigned as described in the literature [18]. To simulate entire plate-surface to bone-surface interface fixation, screw thread contact points at both the plate-screw and screw-bone interfaces were assigned bonding features, while the contact behavior between the bone and calcaneal plate was assigned as frictionless. We constrained the degree of freedom of all nodes of the lower edge of the calcaneus and foot load-bearing area to zero as the boundary conditions. The simplified model was used without considering the influence of ligaments and the pressure friction between the locking plate and the calcaneus. The calcaneus was placed in a neutral position. The calcaneocuboid joint surface and the contact area of the calcaneus to the ground were first fixed in space. A total of 500 N of the load was distributed as follows: at Achilles tendon attachment (Z axis upward), at posterior facet (Z axis, downward), and at anterior and middle facet (Z axis, downward) (Figure 3). ANSYS software was used to analyze and calculate the stress distribution and displacement of the calcaneus fracture fragment and locking plate.
To compare the biomechanical performance of anterior process locking plate combined with percutaneous cannulated screws fixation (screw group) versus anterior process locking plate fixation alone (plate group) for all 3 groups of Sanders type II A, B, and C calcaneal fractures, the outcome was measured based on the criteria below [19].
Results
ESTABLISHMENT AND VALIDATION OF THE CALCANEAL FRACTURE MODEL:
In this study, a finite element calcaneal model consisting of 13 372 units and 25 352 nodes was constructed, and the shape and characteristics of the calcaneus model were analyzed. The calcaneus body length was 72.06 mm, the width was 28.4 mm, the height was 52.1 mm, the Gissane’s angle was 113.4°, and the Bohler’s angle was 34.0°. This is consistent with previously published studies [20,21] indicating that the FEA calcaneus model established is similar to the shape and characteristics of the real calcaneus.
DISPLACEMENT OF FRACTURE FRAGMENTS:
The amount of fracture fragment displacement represents the stability of the fracture. Upon loading the calcaneal fracture models, medial and lateral displacements and relative displacement of the fracture fragment were recorded. In the screw group, for type II A, B, and C calcaneal fractures, the medial displacement of the fracture fragment was 11.262 um, 11.226 um, and 10.491 um, lateral displacement was 11.263 um, 11.230 um, and 10.491 um, and the relative displacement was 1.000 um, 4.000 um, and 0.200 um, respectively. In the plate group, for type A, B, and C calcaneal fractures, the medial displacement of the fracture fragment was 11.602 μm, 11.287 μm, and 10.500 μm, lateral displacement was 11.600 μm, 11.283 μm, and 10.501μm, and the relative displacement was 1.400 μm, 4.300 μm, and 1.000 μm, respectively (Tables 2–4). The fracture displacement in both groups was less than 150 μm, suggesting that both the screw group and the plate group provide good stability and would not be the cause for fracture nonunion or infection.
According to the Sanders classification, based on the fracture line location, type II calcaneal fractures are classified into A, B, and C from lateral to medial. In the plate group, the laterally placed locking provided sufficient stability to the lateral calcaneal fragment but slightly less stability to the medial of the calcaneus, as shown by slightly higher values of medial displacement than lateral displacement (Figure 4A, 4B). In the screw group, in combination with the laterally placed plate, percutaneous cannulated screws were driven from the calcaneal tuberosity toward the calcaneocuboid joint or posterior facet, which provides additional support and stability to the medial fragment, as shown by the decreased medial fragment displacement compared to lateral displacement in type A, B, and C (Figure 4A, 4B). The screw group had better stability, especially to the medial fragment, than the plate group. Moreover, the relative displacement of the fracture fragment in the screw group was significantly smaller than that in the plate group (Figure 4C), indicating that the screw group performed better than the plate group in terms of fixation and reduction maintenance and had better stability.
STRESS ON THE CALCANEAL FRAGMENTS:
When the stress on the fracture fragment exceeds 56 MPa, it triggers bone absorption, which results in loosening of screws and fixation failure. Stress analysis results showed that in all the calcaneal fracture models, the peak stress on the bone fragments did not exceed 56 Mpa. In the screw group, for type II A, B, and C calcaneal fractures, the peak stress was 12.96 MPa, 13.47 MPa, and 14.00 MPa, respectively. In the plate group, for type II A, B, and C calcaneal fractures, the peak stress was 15.02 MPa, 13.036 MPa, and 13.55 MPa, respectively (Tables 2–4). No difference was seen among the cohorts, indicating strong fixation.
The stress distribution graph (Figure 5A) shows no apparent stress-concentrated area (stress concentration indicated in red). However, in the plate group, stress was observed at the calcaneus’s middle and posterior articular surface (Figure 6A). In the screw group, the stress distribution was more dispersed than in the plate group due to the additional support of the medial fragment by the cannulated screws (Figure 6B), showing that the stress distribution on the calcaneus in the screw group was better than that in the plate group after fixation.
STRESS IN THE PLATE AND SCREWS:
According to the Von Mises criterion, when the stress exceeds 600 MPa, the plate will fracture; when the stress exceeds 450 MPa, the plate will undergo permanent deformation. Stress analysis results show that in the screw group, for type II A, B, and C calcaneal fractures, the peak stress maximum stress pressures of the screw group when fixing A, B, and C are 40.53 MPa, 48.12 MPa and 46.27 MPa, respectively. In the plate group, for type II A, B, and C calcaneal fractures, the peak stress was 35.226 MPa, 36.896 MPa, and 66.621 MPa (Tables 2–4). In all the calcaneal fracture models, the peak stress in the plate and screws were within range and did not exceed 450 MPa, and no significant difference in stress on the plate and screws was seen in either cohort.
As seen in Figure 4B, no evident high-stress concentration regions were seen in stress distribution on the plates and screw groups. In the plate group, the stress distribution showed stress distributed in the middle of the plate (the red area appears), suggesting that the middle section of the plate needs to be thickened (Figure 6D). Additionally, in the plate group, the distal end of the screw, which bears the axial load, was more important. In the screw group, the stress distribution was dispersed (no red area) (Figure 6C), indicating that the stress distribution in the plate and screws of the screw group was better than that of the plate group after fixation and provided better stability.
Discussion
The calcaneus bears the weight of the whole body, but it has an uneven density, and the bone trabecula of the body is scarce, so it is prone to fractures when subjected to strong external forces. The anatomical shape of the calcaneus is irregular, and the valgus angle is 0–5°. Failure of fixation causes many complications and leads to operation failure. To better reduce and fix the fracture, ORIF has become a standard surgical method for treating calcaneal fractures in clinical practice. Traditional operative incisions adopted an extended lateral approach. However, scholars such as Mehta et al [22] and others believe that due to the extensive surgical incisions and peeling of the lateral calcaneal flaps, the edge of the incision after the operation has high tension, and necrosis of the skin may cause complications such as wound infection, plate exposure, and osteomyelitis, seriously affecting the prognosis. According to reports in the literature, the incidence of postoperative incision complications for calcaneal fractures with an extended lateral approach is as high as 43% [6].
Currently, minimally invasive locking plates using the invasive sinus tarsi approach are popular among surgeons for treating Sanders type II calcaneal fractures; the operative incision is small, and the incidence of postoperative incision complications is low [9,23,24]. However, the calcaneal shape cannot be directly viewed using this approach, increasing the risk of fixation failure without aid from percutaneous canulated screws, and with less ability to meet the patient’s early weight-bearing needs [25]. The minimally invasive percutaneous plate osteosynthesis (MIPPO) is a small vertical incision placed midway between the fibula’s posterior border and the Achilles tendon’s anterolateral border, followed by percutaneous internal fixation; however, this technique is suitable for moderately displaced calcaneal fractures or non-comminuted calcaneus fractures due to limited fixation strength [6,26]. Percutaneous canulated screws fixation offers minimal incision, shorter operation time and hospital stay time, less blood loss, and better visual analog scale (VAS) scores; however, they are not as strong as plating and can result in fracture displacements [27]. It is unknown whether adding percutaneous cannulated screws with an anterior process locking plate can strengthen the stability of the fracture and reduce stress on the plate fixation, and this requires further research to shed light on this clinical challenge.
Our experiment used the finite element analysis method to study the mechanical stability of the Sanders type II calcaneal fractures model fixed by the screw and plate groups. We found that the screw and plate groups could achieve appropriate mechanical stability for the Sanders type II calcaneal fractures. Furthermore, the stability of the screw group is better than that of the plate group. The above results indicate that for Sanders subtypes II of calcaneal fractures, the 2 fixation methods can restore the flatness of the articular surface and maintain the fixation strength within a reasonable range, have a good fixation effect, and can meet the needs of patients for early weight-bearing functional exercise. The long auxiliary screws can enhance stability and achieve multi-planar and multidimensional fixation. Moreover, they can fix the calcaneus’s secondary fracture line, and the fixation is further stabilized and the stress is equally distributed. Shi et al also found that the additional 2 screws have a decisive effect on maintaining the entire calcaneal force line and the stability of the medial column and posterior articular surface [25]. Delmon et al reported that balloon calcaneoplasty combined with lateral screw osteosynthesis for the treatment of Sanders 2B calcaneal fracture is comparable to a locking plate regarding displacement and stress distribution [28–30].
This study has some limitations. Firstly, finite element analysis places little emphasis on the complex structural differences in human tissues, relying only on CT to build models and not considering the human foot’s complex dynamic changes. Secondly, our study lacks weight-bearing CT scan model and gait analysis studies to better evaluate the biomechanical stability of calcaneal fractures. Therefore, this experiment is a preliminary study analyzing the internal fixation of calcaneal fractures. Further biomechanical study of cadaveric specimens is needed to provide supporting evidence for clinical application.
Conclusions
For Sanders type II calcaneal fractures of all subtypes, the screw group had better stability than the plate group. Both fixation methods were within a reasonable range for restoring the levelling effect of the joint surface and maintaining the strength of fixation, and both had good mechanical stability. Finite element analysis is reliable, and biomechanics and clinical studies are needed to verify the experimental results.
Figures
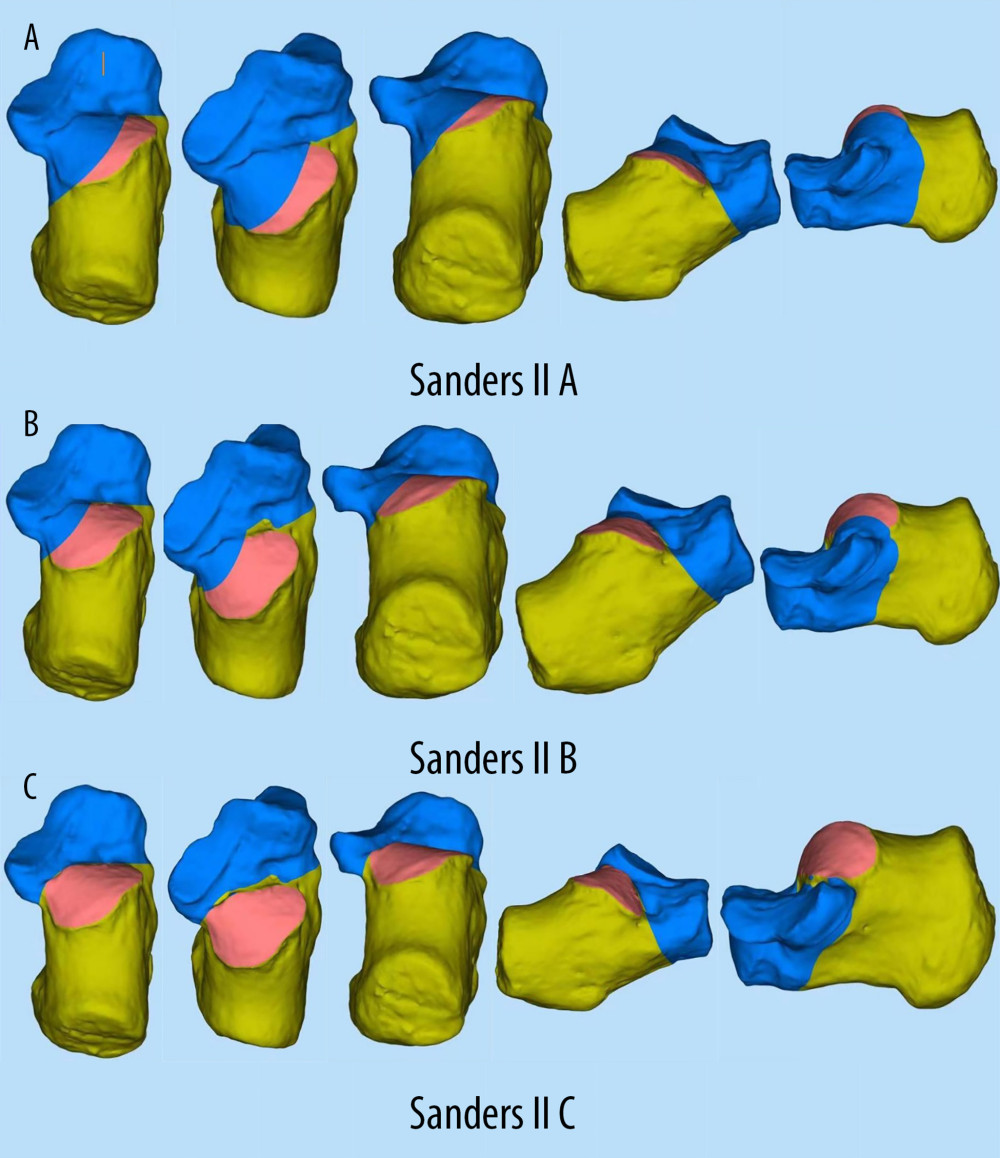 Figure 1. (A–C)3D model of Sanders type II calcaneal fracture.
Figure 1. (A–C)3D model of Sanders type II calcaneal fracture. 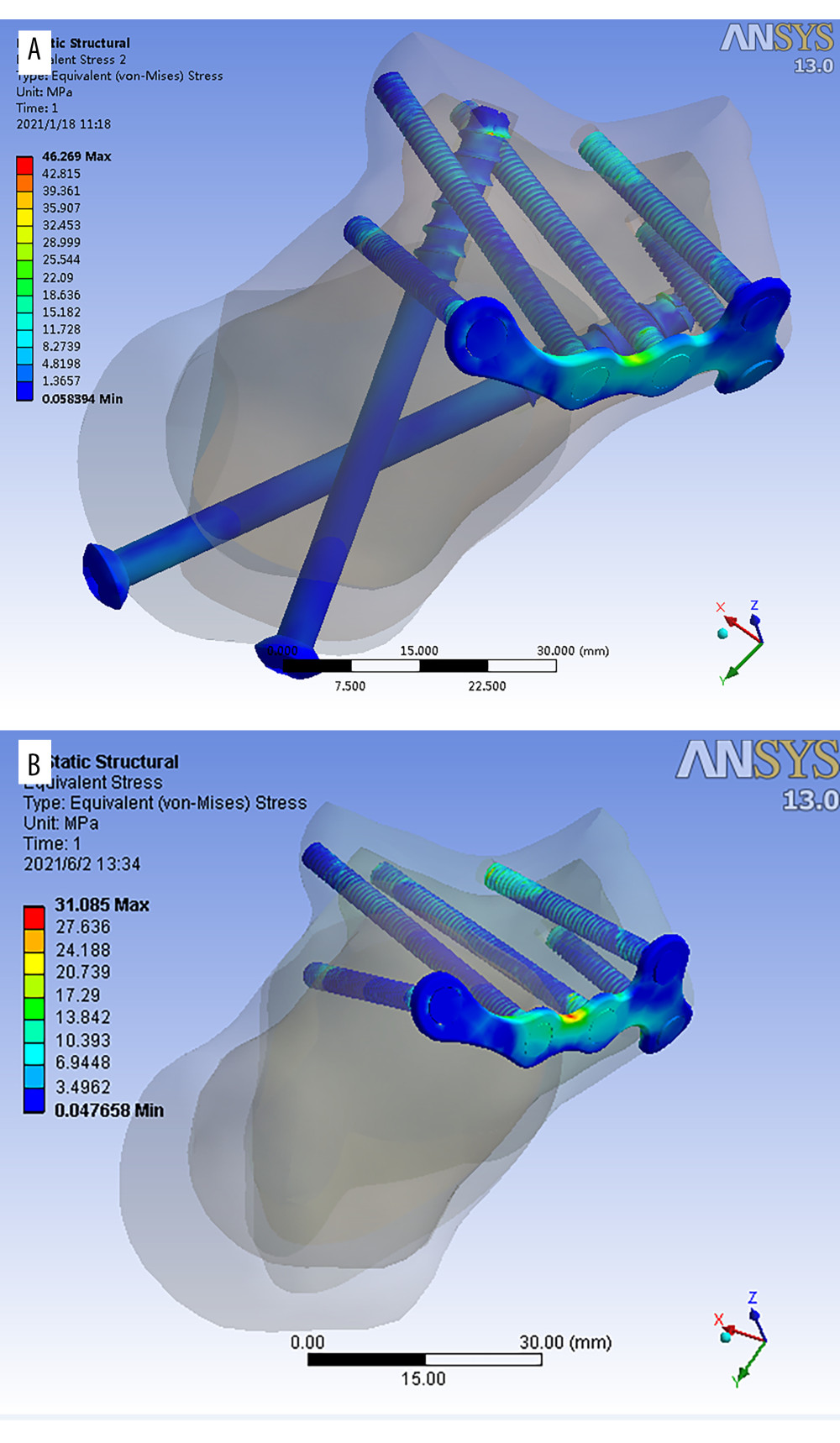 Figure 2. (A, B) 3D model of minimally invasive internal fixation system for Sanders type II calcaneal fracture. (A – simple minimally invasive plate. B – minimally invasive plate with long screws from posterior to anterior).
Figure 2. (A, B) 3D model of minimally invasive internal fixation system for Sanders type II calcaneal fracture. (A – simple minimally invasive plate. B – minimally invasive plate with long screws from posterior to anterior). 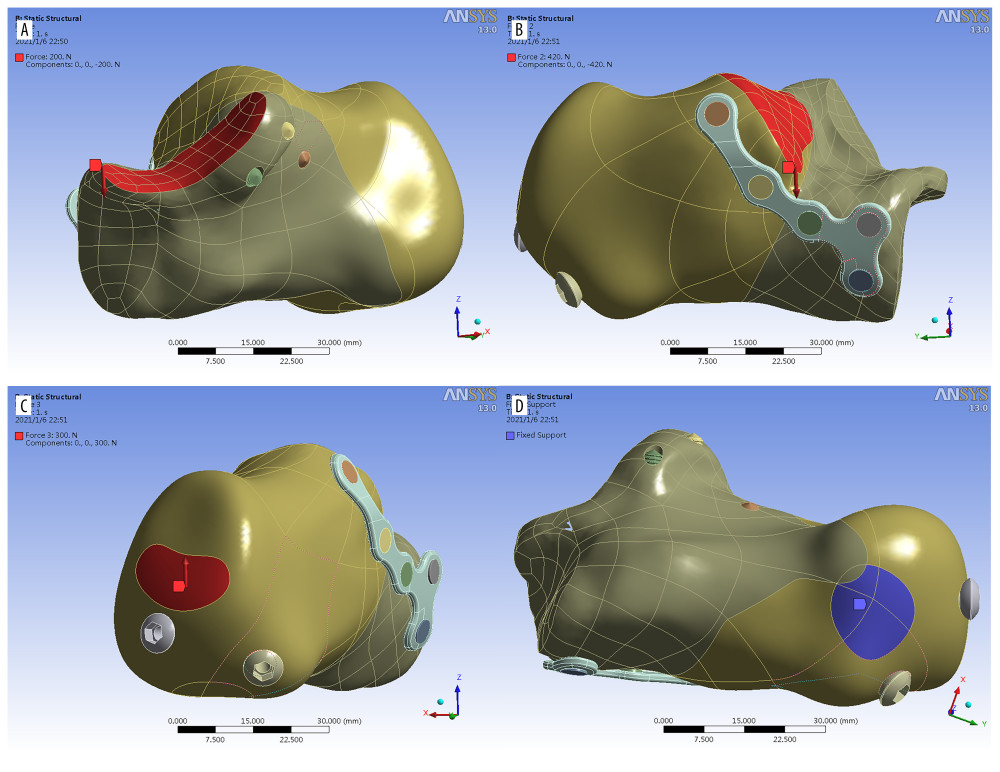 Figure 3. Load distribution A) red area: at posterior facet (Z axis, downward), B) red area: anterior and middle facet (Z axis, downward), C) red area: Achilles tendon attachment (Z axis upward), D) Blue area: Fixed contact area of the calcaneus to the ground.
Figure 3. Load distribution A) red area: at posterior facet (Z axis, downward), B) red area: anterior and middle facet (Z axis, downward), C) red area: Achilles tendon attachment (Z axis upward), D) Blue area: Fixed contact area of the calcaneus to the ground. 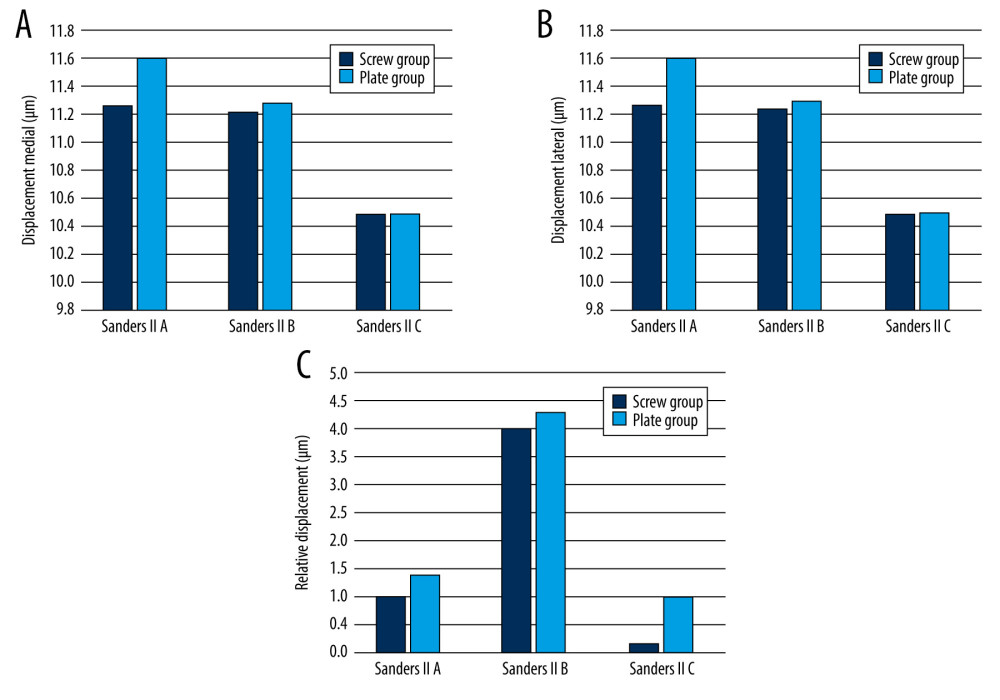 Figure 4. Histogram representing displacement medial (A), lateral (B) and relative displacement (C) of the fracture fragments in Sanders type II A, B, C fixed by the screw group and the plate group.
Figure 4. Histogram representing displacement medial (A), lateral (B) and relative displacement (C) of the fracture fragments in Sanders type II A, B, C fixed by the screw group and the plate group. 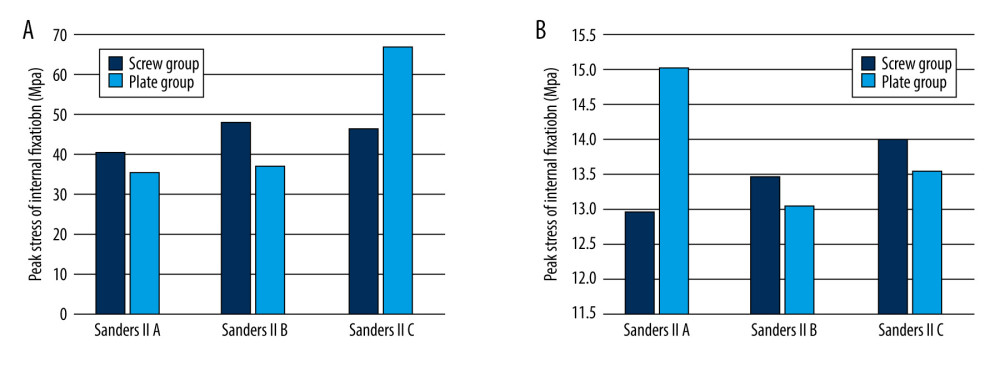 Figure 5. Histogram representing peak stress on fracture fragment (A) and peak stress on internal fixation (B) in Sanders type II A, B, C fracture fixed by the screw and plate groups.
Figure 5. Histogram representing peak stress on fracture fragment (A) and peak stress on internal fixation (B) in Sanders type II A, B, C fracture fixed by the screw and plate groups. 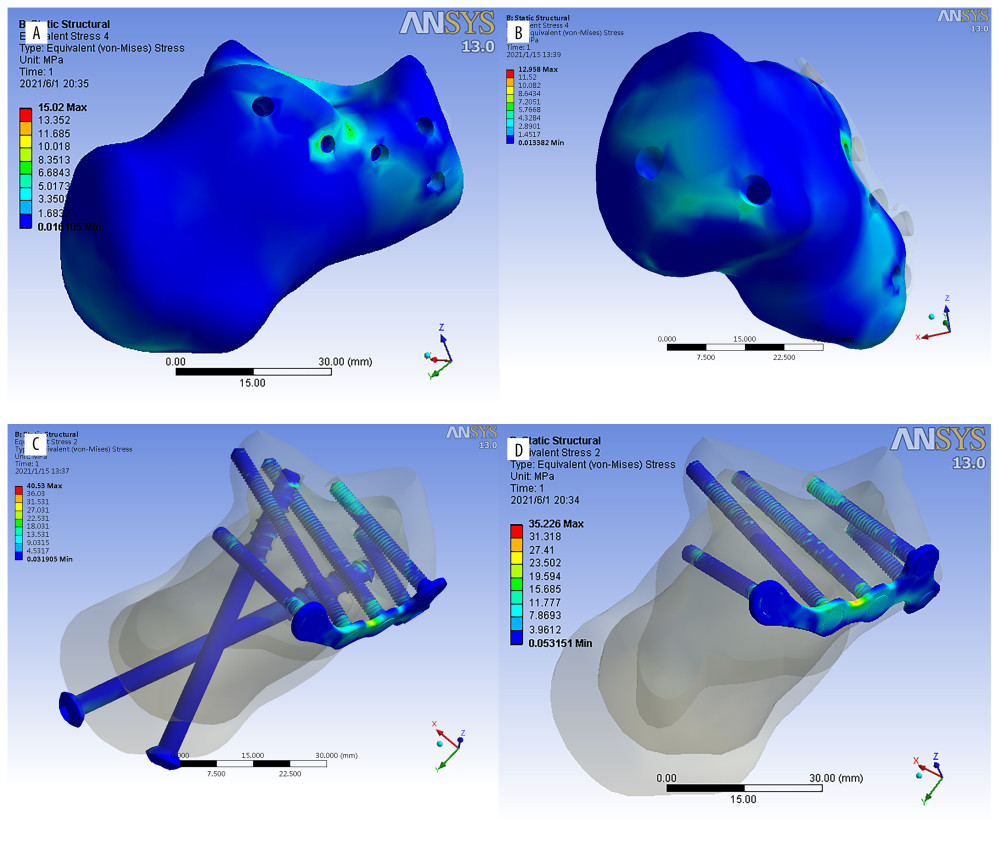 Figure 6. (A–D) Stress distribution diagrams of Sanders type II A, B, and C calcaneal fractures.
Figure 6. (A–D) Stress distribution diagrams of Sanders type II A, B, and C calcaneal fractures. Tables
Table 1. Value of cortical and cancellous bones and titanium (titanium was used in all implant conditions, including the locking plate, fixation screws and percutaneous cannulated screws).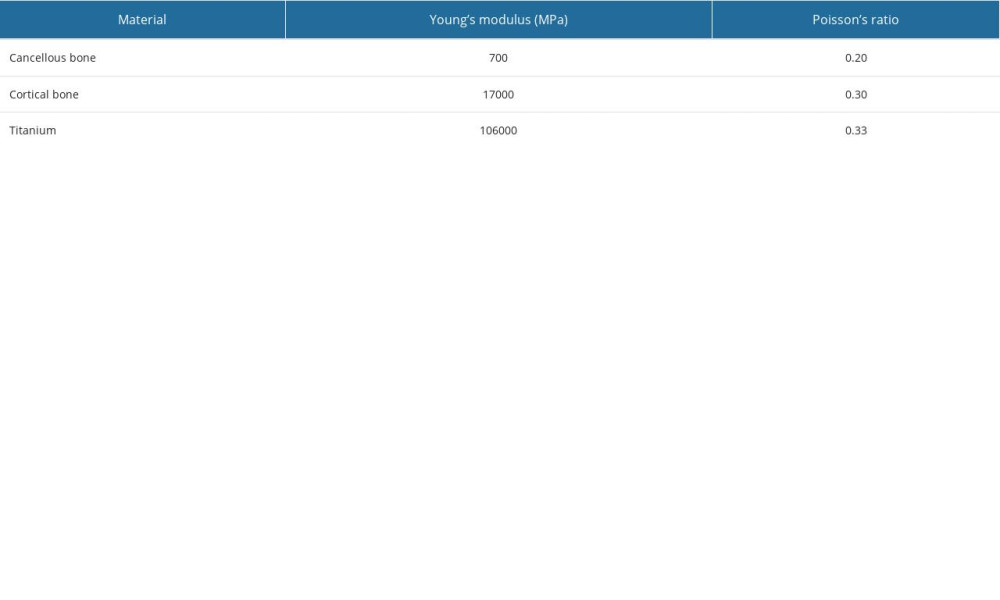 Table 2. Finite element analysis results of Sanders type II A calcaneal fractures.
Table 2. Finite element analysis results of Sanders type II A calcaneal fractures.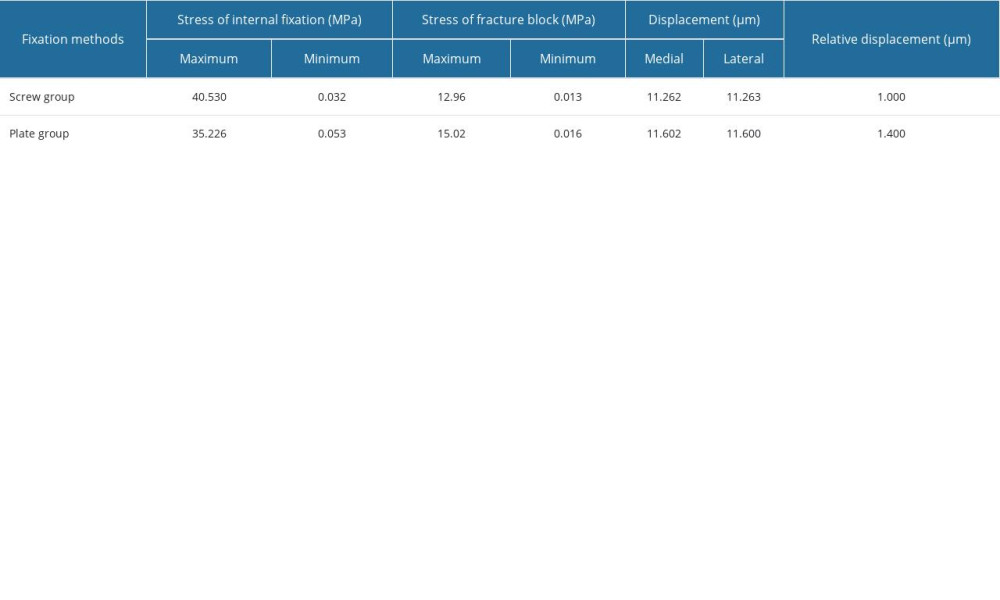 Table 3. Finite element analysis results of Sanders type II B calcaneal fractures.
Table 3. Finite element analysis results of Sanders type II B calcaneal fractures.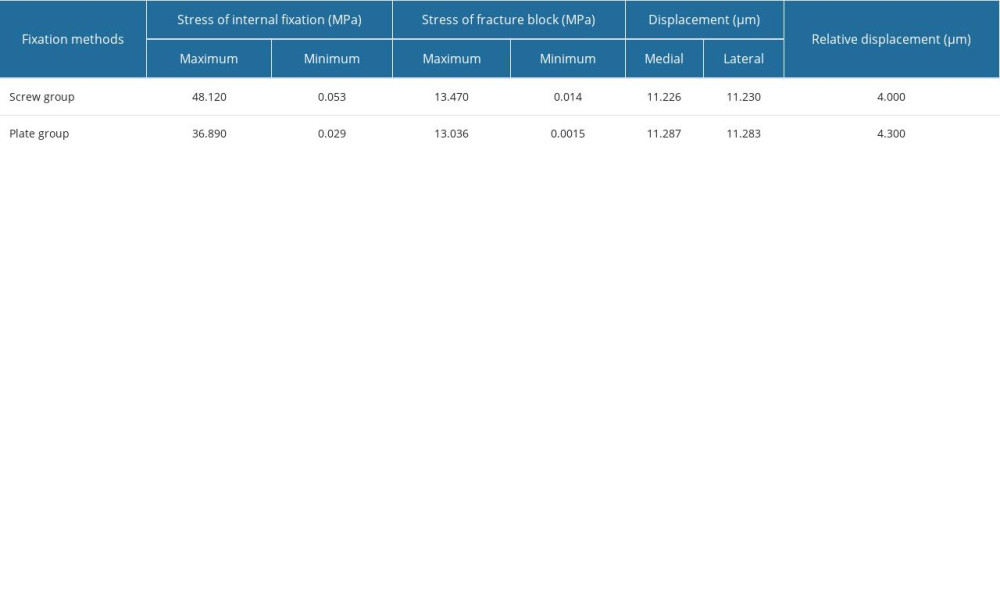 Table 4. Finite element analysis results of Sanders type II C calcaneal fractures.
Table 4. Finite element analysis results of Sanders type II C calcaneal fractures.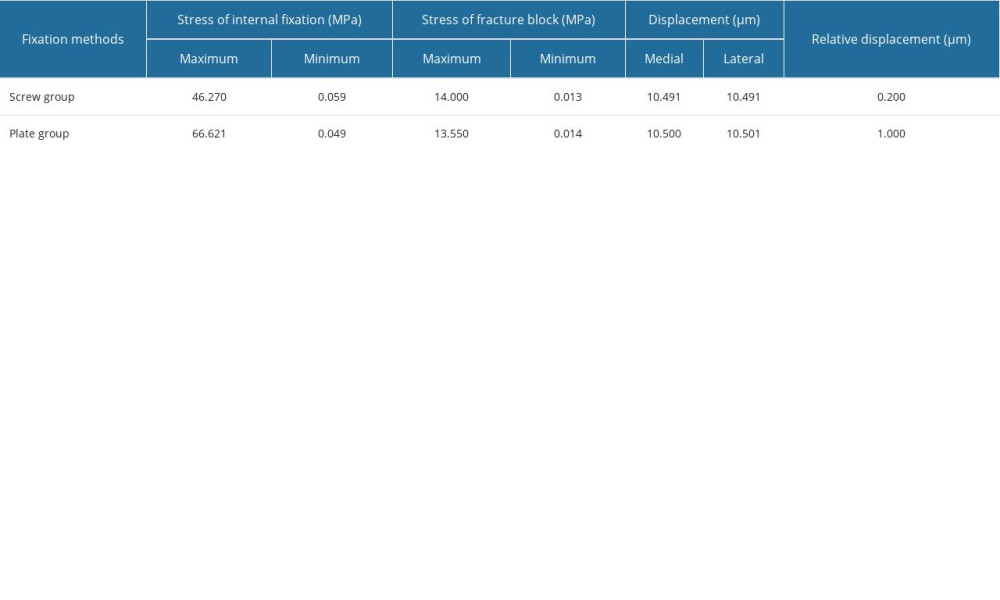
References
1. Wallin KJ, Cozzetto D, Russell L, Evidence-based rationale for percutaneous fixation technique of displaced intra-articular calcaneal fractures: A systematic review of clinical outcomes: J Foot Ankle Surg, 2014; 53(6); 740-43
2. Pflüger P, Zyskowski M, Greve F, Patient-reported outcome following operative and conservative treatment of calcaneal fractures: A retrospective analysis of 79 patients at short-to midterm follow-up: Frontiers in Surgery, 2021; 8; 620694
3. Epstein N, Chandran S, Chou L, Current concepts review: Intra-articular fractures of the calcaneus: Foot Ankle Int, 2012; 33(1); 79-86
4. Pelliccioni AAA, Bittar CK, Zabeu JLA, Surgical treatment of intraarticular calcaneous fractures of Sanders’ types II and III: Systematic review: Acta Ortop Bras, 2012; 20; 39-42
5. Guerado E, Bertrand ML, Cano JR, Management of calcaneal fractures: What have we learnt over the years?: Injury, 2012; 43(10); 1640-50
6. Jin C, Weng D, Yang W, Minimally invasive percutaneous osteosynthesis versus ORIF for Sanders type II and III calcaneal fractures: A prospective, randomized intervention trial: J Orthop Surg Res, 2017; 12(1); 10
7. Ahn J, Kim TY, Kim TW, Jeong BO, Learning curve for open reduction and internal fixation of displaced intra-articular calcaneal fracture by extensile lateral approach using the cumulative summation control chart: Foot Ankle Int, 2019; 40(9); 1052-59
8. Bai L, Hou Y-L, Lin G-H, Sinus tarsi approach (STA) versus extensile lateral approach (ELA) for treatment of closed displaced intra-articular calcaneal fractures (DIACF): A meta-analysis: Orthop Traumatol Surg Res, 2018; 104(2); 239-44
9. Park CH, Lee DY, Surgical treatment of sanders type 2 calcaneal fractures using a sinus tarsi approach: Indian J Orthop, 2017; 51(4); 461-67
10. Qiang Mf, Singh RK, Chen Yx, Computational biomechanical analysis of postoperative calcaneal fractures with different placement of the sustentaculum screw: Orthop Surg, 2020; 12(2); 661-67
11. Ouyang H, Deng Y, Xie P, Biomechanical comparison of conventional and optimised locking plates for the fixation of intraarticular calcaneal fractures: A finite element analysis: Comput Methods Biomech Biomed Engin, 2017; 20(12); 1339-49
12. Ni M, Wong DW-C, Mei J, Biomechanical comparison of locking plate and crossing metallic and absorbable screws fixations for intra-articular calcaneal fractures: Sci China Life Sci, 2016; 59(9); 958-64
13. Li H, Chen Y, Qiang M, Computational biomechanical analysis of postoperative inferior tibiofibular syndesmosis: A modified modeling method: Comp Methods Biomech Biomed Engin, 2018; 21(5); 427-35
14. Pînzaru RM, Pavăl SD, Per ea M: J Pers Med, 2023; 13(4); 587
15. Huang H, Feng Z, Wang W, Finite element analysis of femoral neck fracture treated with Bidirectional compression-Limited Sliding screw: Med Sci Monit, 2021; 27; e929163
16. Wang C, He X, Zhang Z, Three-dimensional finite element analysis and biomechanical analysis of midfoot von mises stress levels in Flatfoot, Clubfoot, and Lisfranc Joint Injury: Med Sci Monit, 2021; 27; e931969
17. Wang H, Wang X, Chen W, Biomechanical comparison of interspinous distraction device and facet screw fixation system on the motion of lumbar spine: A finite element analysis: Chin Med J (Engl), 2014; 127(11); 2078-84
18. Sowmianarayanan S, Chandrasekaran A, Kumar RK, Finite element analysis of a subtrochanteric fractured femur with dynamic hip screw, dynamic condylar screw, and proximal femur nail implants – a comparative study: Proc Inst Mech Eng H, 2008; 222(1); 117-27
19. Vajgel A, Camargo IB, Willmersdorf RB, Comparative finite element analysis of the biomechanical stability of 2.0 fixation plates in atrophic mandibular fractures: J Oral Maxillofac Surg, 2013; 71(2); 335-42
20. Idram I, Lai J-Y, Lee P-Y, A reliable method for morphological measurement of 3D calcaneus models from computed tomography images: Biomed Res, 2019; 30(1); 149-59
21. Meng Z, Wu L, Sun X-l, Gong Z-m, Clinical significance of spiral CT three-dimensional reconstruction for measurement of Chinese calcaneal data: Chinese Journal of Tissue Engineering Research, 2014; 18(20); 3207
22. Mehta CR, An VV, Phan K, Extensile lateral versus sinus tarsi approach for displaced, intra-articular calcaneal fractures: A meta-analysis: J Orthop Surg Res, 2018; 13(1); 243
23. Park J, Che JH, The sinus tarsi approach in displaced intra-articular calcaneal fractures: Arch Orthop Trauma Surg, 2017; 137(8); 1055-65
24. Ma C, Zhao J, Zhang Y, Comparison of the modified sinus tarsi approach versus the extensile lateral approach for displaced intra-articular calcaneal fractures: Ann Transl Med, 2021; 9(8); 695
25. Shi Z, Gu WSurgical management of intra-articular calcaneal fractures: Our misunderstandings: Zhonghua Yi Xue Za Zhi, 2019; 99(21); 1604-7 [in Chinese]
26. Ganie PA, Bhat MA, Mir WA: Operative management of calcaneal fractures using Mippo technique, 2020
27. Cao Y, Xu X, Guo Y, Percutaneous cannulated screw fixation vs. plating with minimally invasive longitudinal approach after closed reduction for intra-articular tongue-type calcaneal fractures: A retrospective cohort study: Front Surg, 2022; 9; 854210
28. He K, Fu S, Liu S, Comparisons in finite element analysis of minimally invasive, locking, and non-locking plates systems used in treating calcaneal fractures of Sanders type II and type III: Chin Med J (Engl), 2014; 127(22); 3894-901
29. Delmon R, Vendeuvre T, Pries P, Percutaneous balloon calcaneoplasty versus open reduction and internal fixation (ORIF) for intraarticular SANDERS 2B calcaneal fracture: Comparison of primary stability using a finite element method: Injury, 2023 [Online ahead of print]
30. Gefen A, Megido-Ravid M, Itzchak Y, Arcan M, Biomechanical analysis of the three-dimensional foot structure during gait: A basic tool for clinical applications: J Biomech Eng, 2000; 122(6); 630-39
Figures
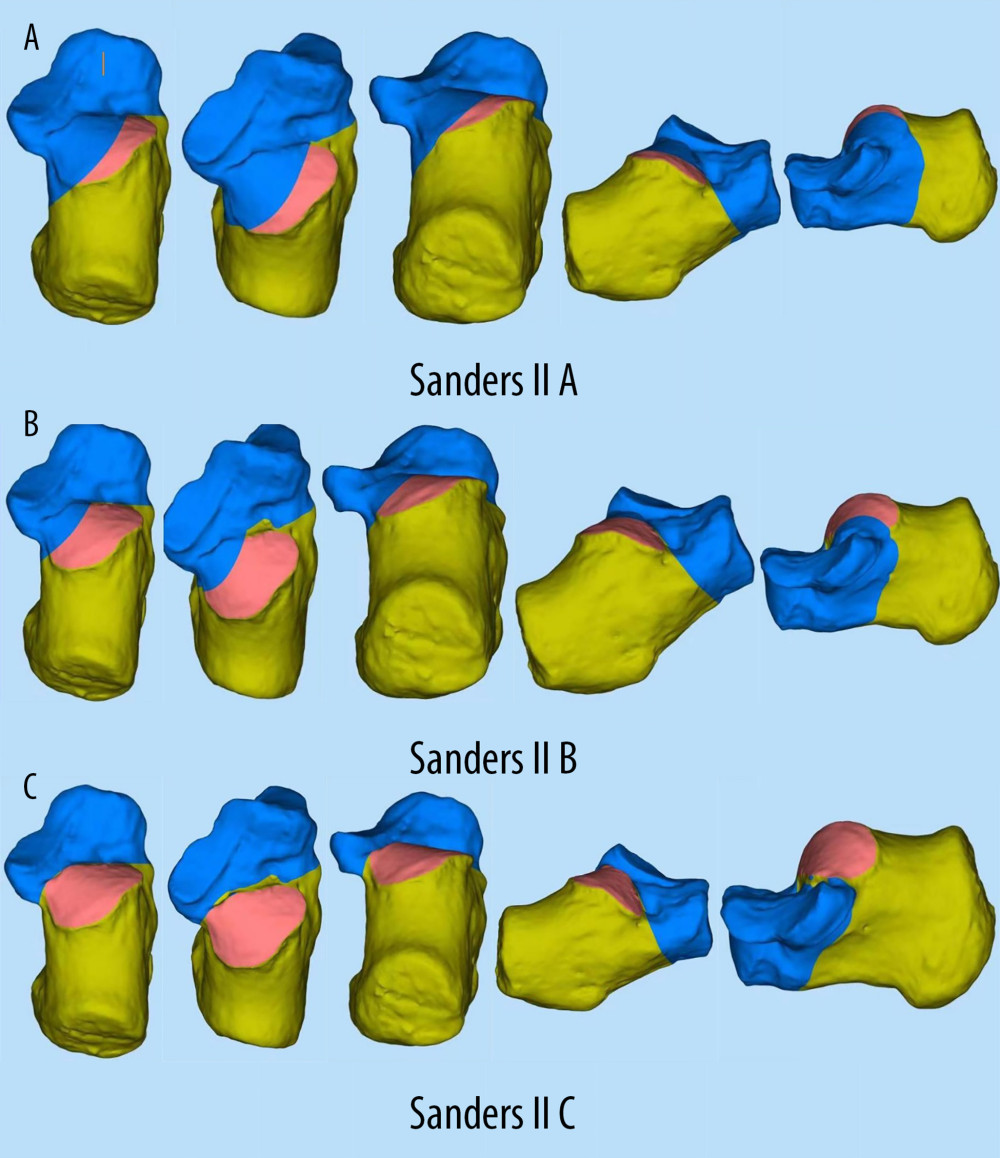 Figure 1. (A–C)3D model of Sanders type II calcaneal fracture.
Figure 1. (A–C)3D model of Sanders type II calcaneal fracture.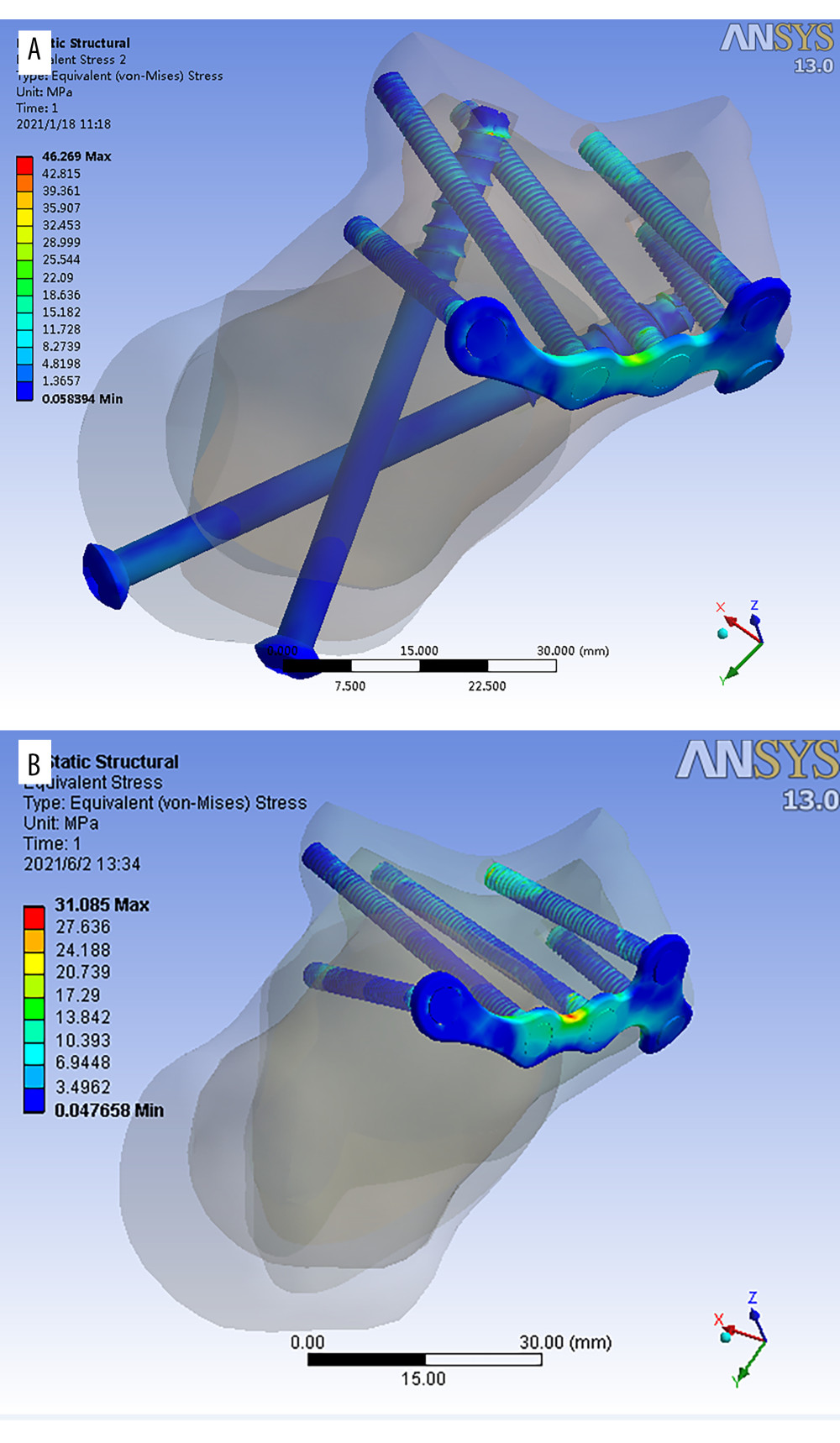 Figure 2. (A, B) 3D model of minimally invasive internal fixation system for Sanders type II calcaneal fracture. (A – simple minimally invasive plate. B – minimally invasive plate with long screws from posterior to anterior).
Figure 2. (A, B) 3D model of minimally invasive internal fixation system for Sanders type II calcaneal fracture. (A – simple minimally invasive plate. B – minimally invasive plate with long screws from posterior to anterior).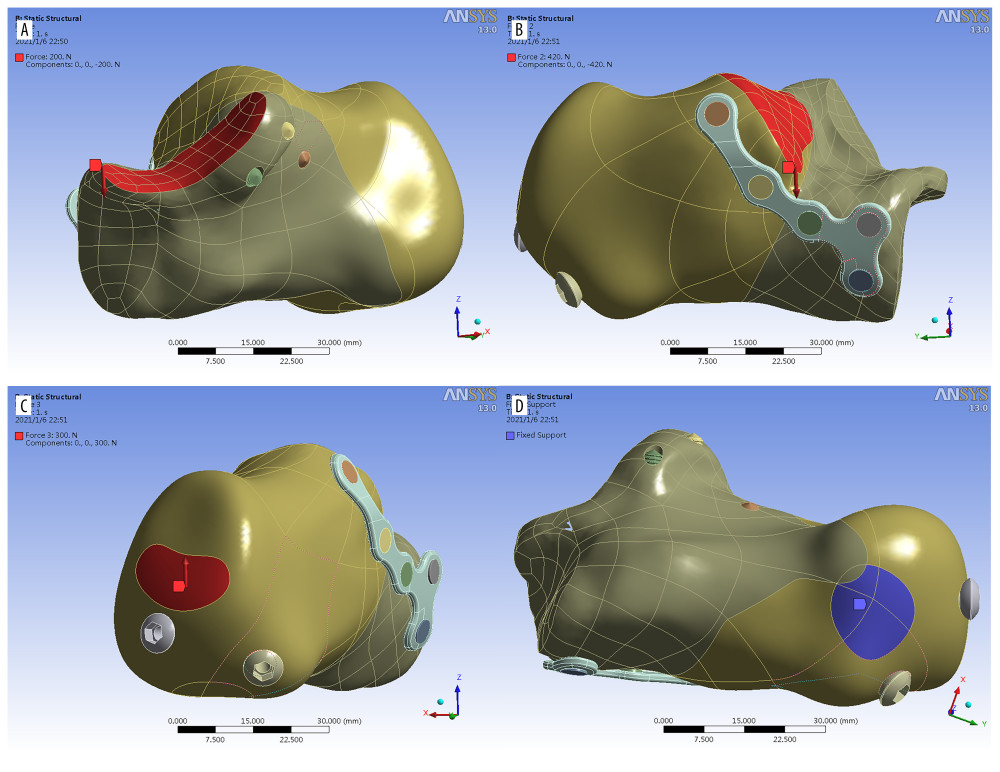 Figure 3. Load distribution A) red area: at posterior facet (Z axis, downward), B) red area: anterior and middle facet (Z axis, downward), C) red area: Achilles tendon attachment (Z axis upward), D) Blue area: Fixed contact area of the calcaneus to the ground.
Figure 3. Load distribution A) red area: at posterior facet (Z axis, downward), B) red area: anterior and middle facet (Z axis, downward), C) red area: Achilles tendon attachment (Z axis upward), D) Blue area: Fixed contact area of the calcaneus to the ground.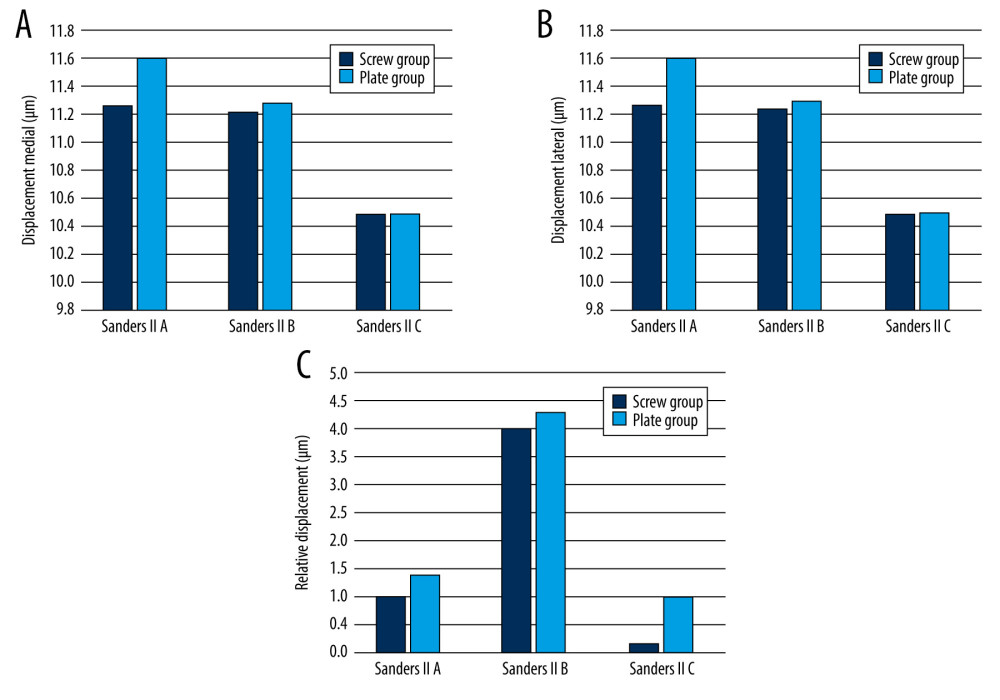 Figure 4. Histogram representing displacement medial (A), lateral (B) and relative displacement (C) of the fracture fragments in Sanders type II A, B, C fixed by the screw group and the plate group.
Figure 4. Histogram representing displacement medial (A), lateral (B) and relative displacement (C) of the fracture fragments in Sanders type II A, B, C fixed by the screw group and the plate group.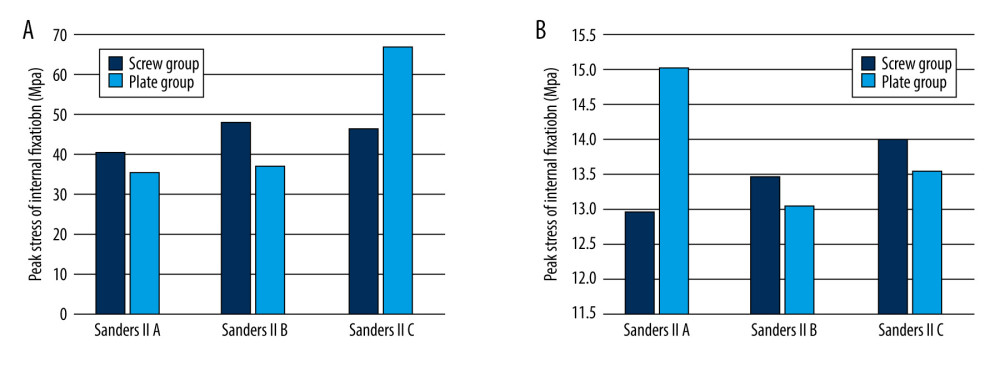 Figure 5. Histogram representing peak stress on fracture fragment (A) and peak stress on internal fixation (B) in Sanders type II A, B, C fracture fixed by the screw and plate groups.
Figure 5. Histogram representing peak stress on fracture fragment (A) and peak stress on internal fixation (B) in Sanders type II A, B, C fracture fixed by the screw and plate groups.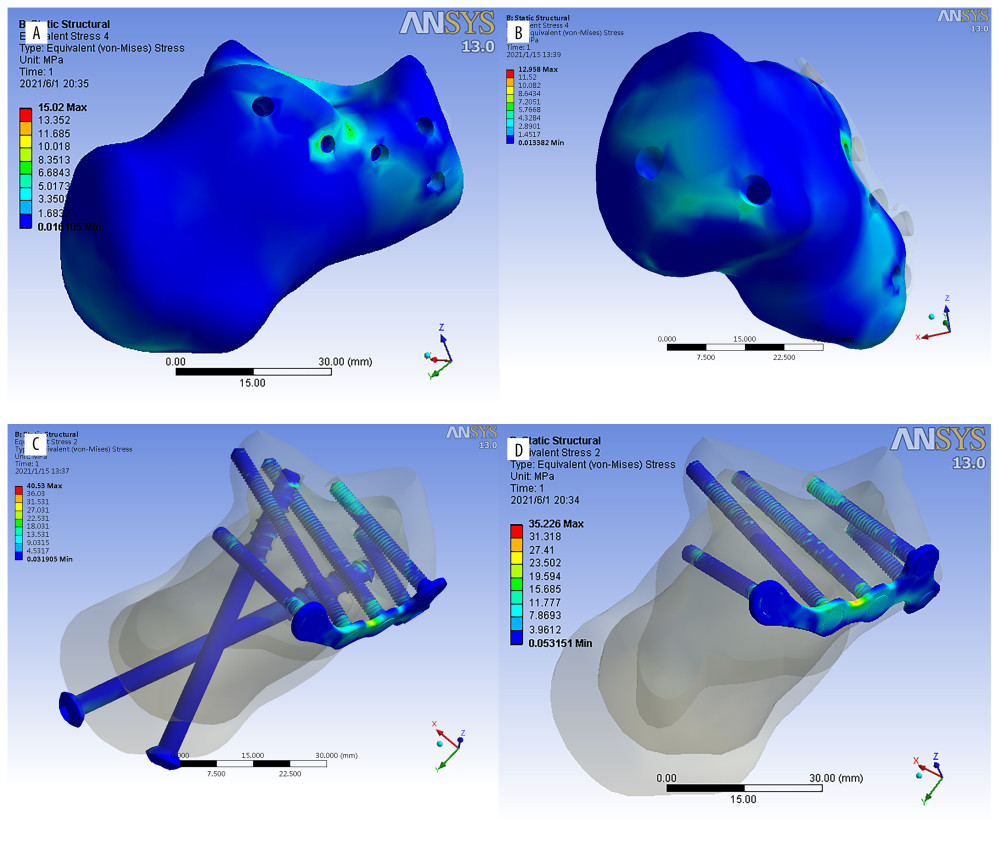 Figure 6. (A–D) Stress distribution diagrams of Sanders type II A, B, and C calcaneal fractures.
Figure 6. (A–D) Stress distribution diagrams of Sanders type II A, B, and C calcaneal fractures. Tables
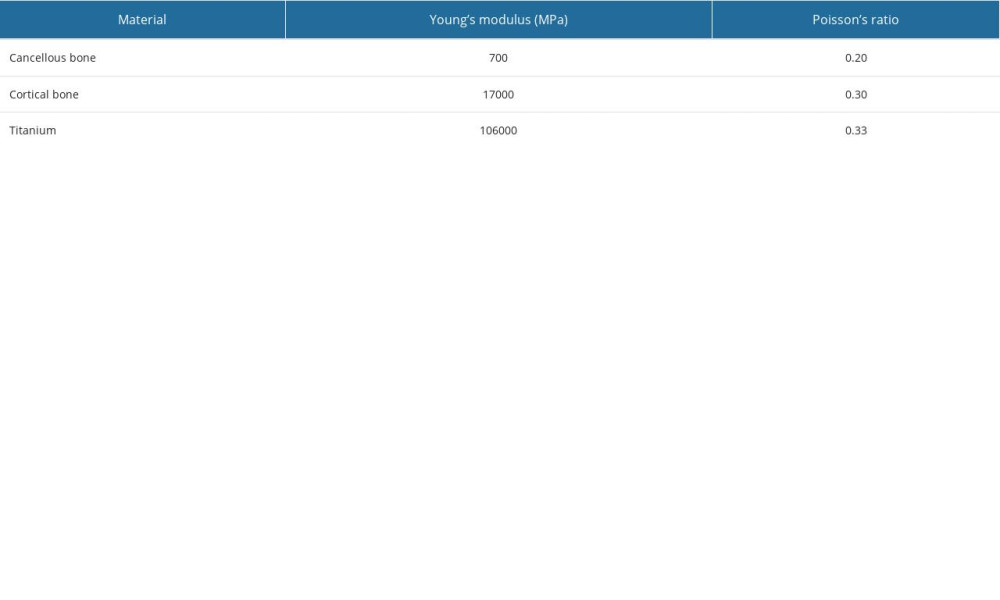 Table 1. Value of cortical and cancellous bones and titanium (titanium was used in all implant conditions, including the locking plate, fixation screws and percutaneous cannulated screws).
Table 1. Value of cortical and cancellous bones and titanium (titanium was used in all implant conditions, including the locking plate, fixation screws and percutaneous cannulated screws).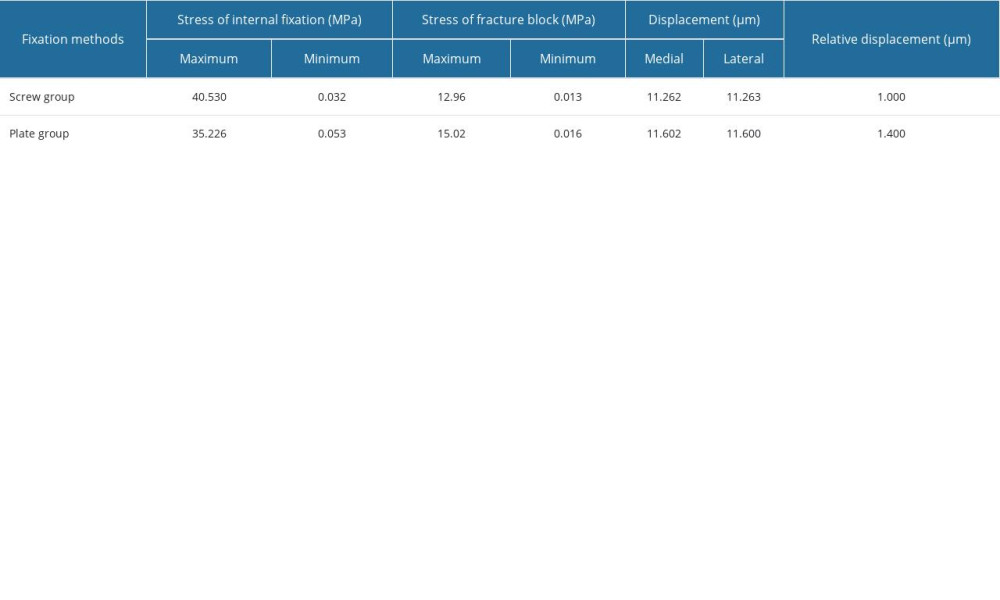 Table 2. Finite element analysis results of Sanders type II A calcaneal fractures.
Table 2. Finite element analysis results of Sanders type II A calcaneal fractures.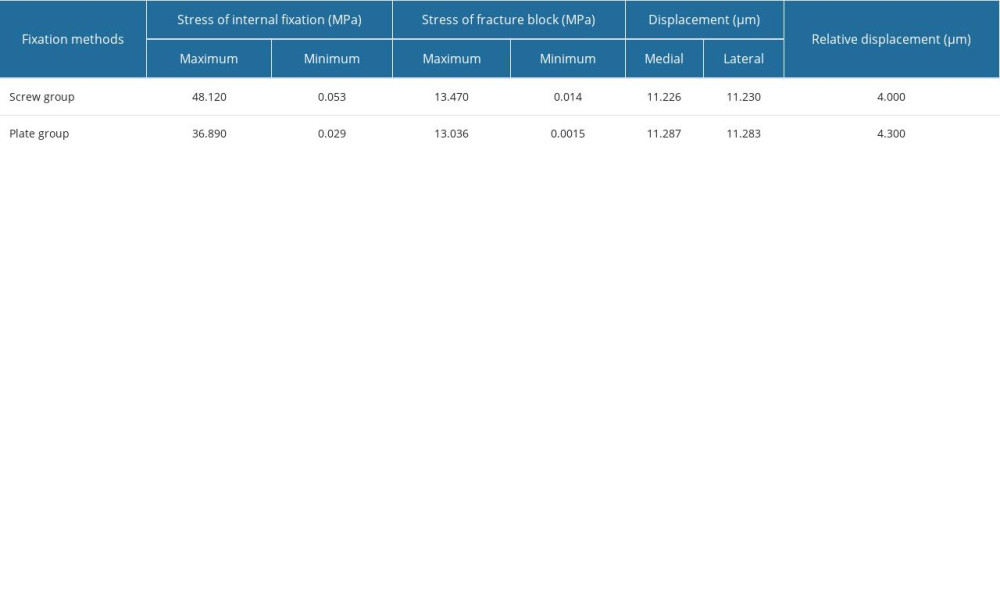 Table 3. Finite element analysis results of Sanders type II B calcaneal fractures.
Table 3. Finite element analysis results of Sanders type II B calcaneal fractures.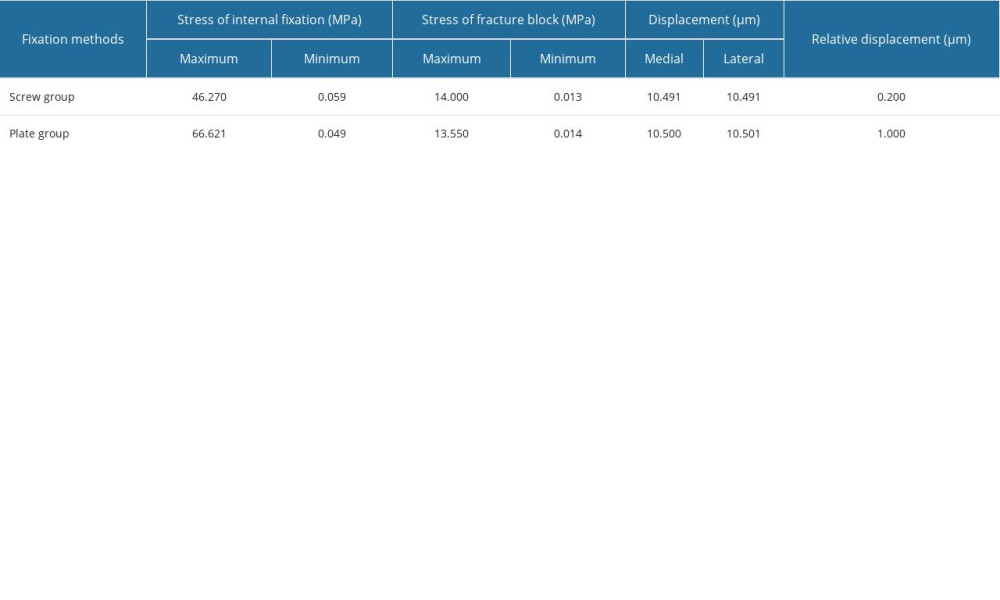 Table 4. Finite element analysis results of Sanders type II C calcaneal fractures.
Table 4. Finite element analysis results of Sanders type II C calcaneal fractures.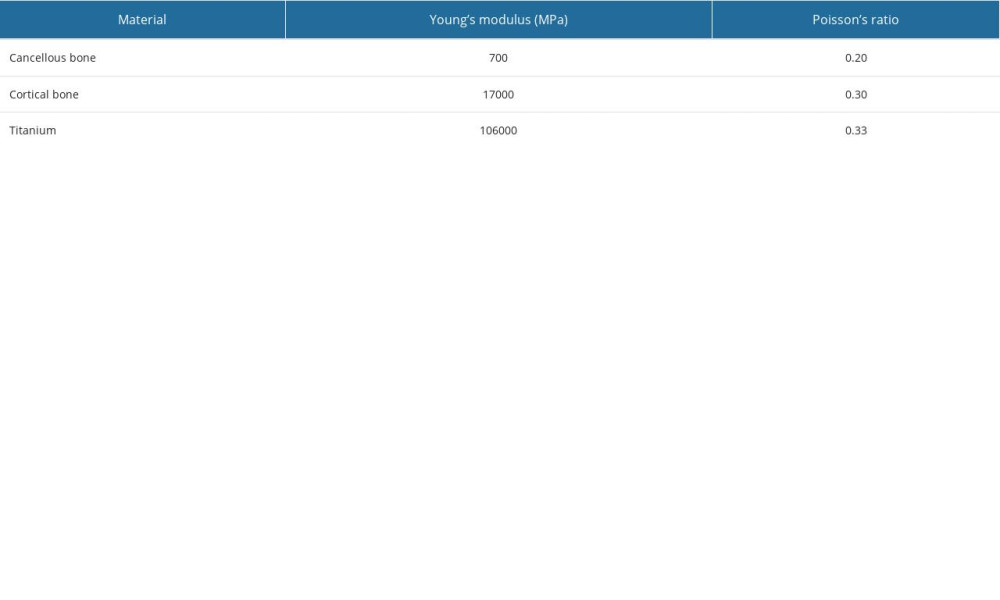 Table 1. Value of cortical and cancellous bones and titanium (titanium was used in all implant conditions, including the locking plate, fixation screws and percutaneous cannulated screws).
Table 1. Value of cortical and cancellous bones and titanium (titanium was used in all implant conditions, including the locking plate, fixation screws and percutaneous cannulated screws).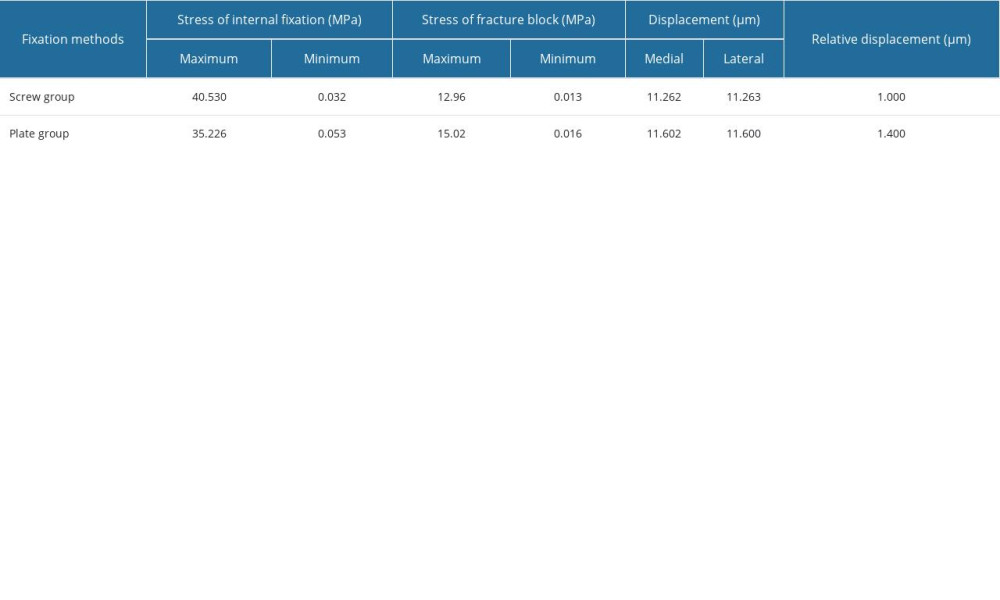 Table 2. Finite element analysis results of Sanders type II A calcaneal fractures.
Table 2. Finite element analysis results of Sanders type II A calcaneal fractures.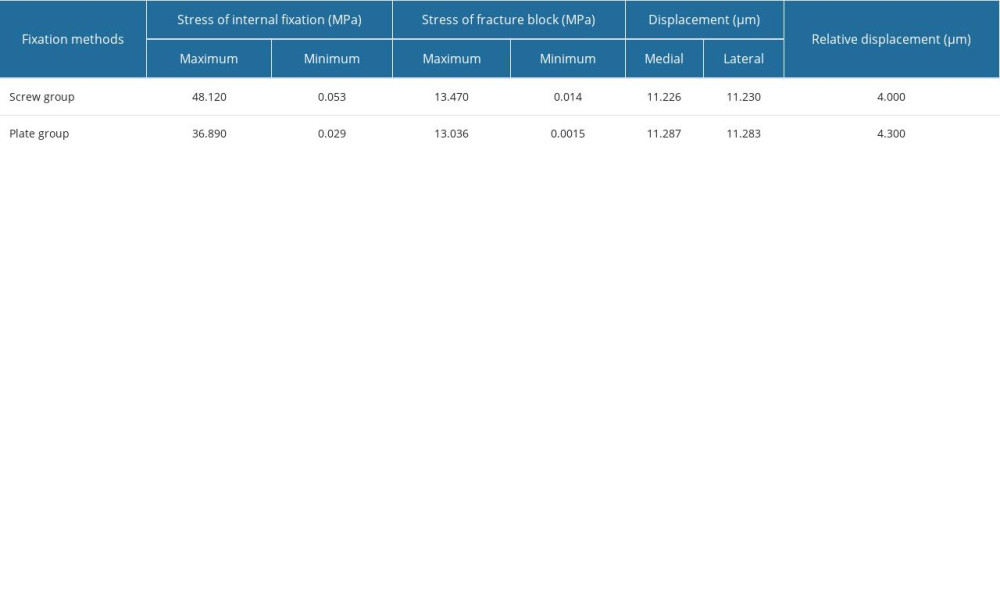 Table 3. Finite element analysis results of Sanders type II B calcaneal fractures.
Table 3. Finite element analysis results of Sanders type II B calcaneal fractures.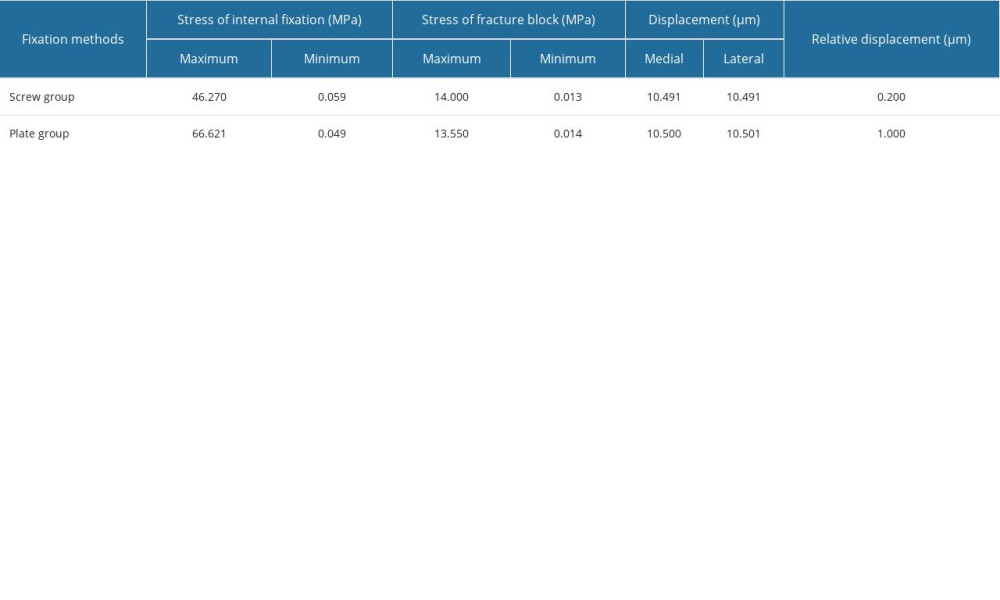 Table 4. Finite element analysis results of Sanders type II C calcaneal fractures.
Table 4. Finite element analysis results of Sanders type II C calcaneal fractures. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








