26 October 2023: Clinical Research
Identifying Predominant Causes of Death Among Hospitalized COVID-19 Patients During Poland’s Second and Third Waves
Irina NiecwietajewaDOI: 10.12659/MSM.941455
Med Sci Monit 2023; 29:e941455
Abstract
BACKGROUND: Number of confirmed COVID-19 deaths per million population in Poland between November 2020 and May 2021 was one of the largest in Europe. This retrospective study was conducted at a single center in Poland between November 2020 and May 2021to evaluate the morbidity and mortality rates in 581 patients hospitalized with COVID-19.
MATERIAL AND METHODS: A retrospective single-center study was conducted in a dedicated COVID-19 hospital from November, 2020 to May, 2021. The data of 581 hospitalized patients were analyzed. Multimorbidity was assessed using the Charlson Comorbidity Index, including chronic kidney, respiratory, cardiovascular diseases, diabetes mellitus, cancer, and dementia. The observation period covered admission to the hospital for severe COVID-19 until discharge or death. Diagnosis of COVID-19 was confirmed by quantitative reverse transcription polymerase chain reaction test. Statistical analysis was carried out in the IBM SPSS Statistics program.
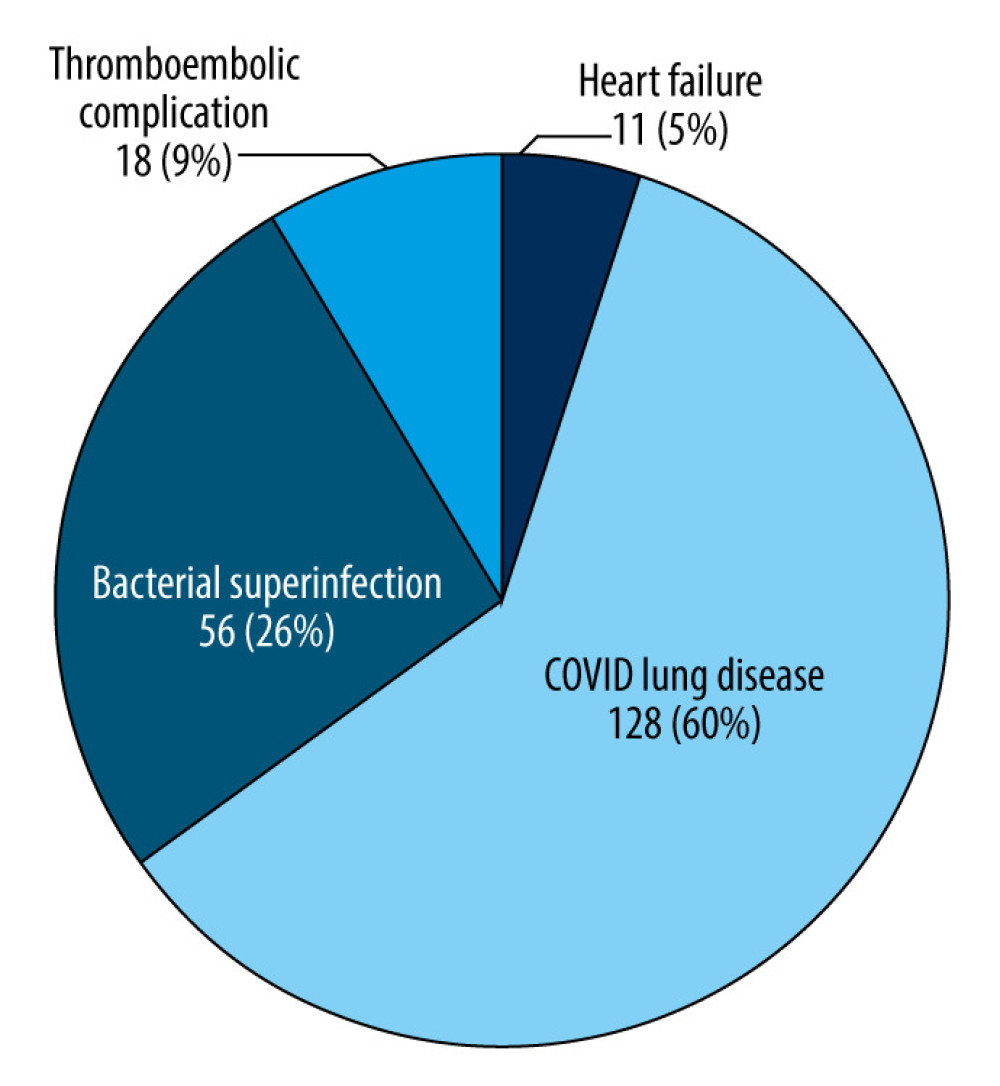
RESULTS: The mortality rate was 35% of all admitted patients. Lung damage was the cause of death in 60%, bacterial superinfection in 26%, arterial thrombosis or thromboembolism in 9%, and heart failure in 5% of patients. The chi-square test showed a significant relationship between sex and the cause of death related to COVID-19 pneumonia and bacterial ventilator-associated pneumonia (VAP).
CONCLUSIONS: The findings from this study supports findings from other countries that between November 2020 and May 2021, before SARS-CoV-2 vaccination programs were fully implemented and before effective medications and antiviral agents were developed, patients with severe COVID-19 had high rates of morbidity and mortality.
Keywords: COVID-19, Cause of Death, Comorbidity, Inpatients, Humans, COVID-19, Retrospective Studies, SARS-CoV-2, COVID-19 Vaccines, Poland
Background
The first case of COVID-19 in Poland was confirmed on March 4, 2020. In the first wave of the pandemic (from March to September 2020), the weekly number of new cases never exceeded 0.2 per 1 million inhabitants. After September 2020, there was a significant increase in new confirmed cases and deaths due to COVID-19. The second and third waves of the pandemic took place in Poland from mid-September 2020 to early June 2021 [1].
These overlapping waves had the highest number of daily confirmed cases, the highest number of hospitalizations, and the highest number of deaths from COVID-19. The present study analyzed data from patients admitted to a multi-specialty hospital temporarily transformed into an infectious disease hospital for the treatment of COVID-19 from October 24, 2020 to May 31, 2021.
The maximum effective reproduction rate (R) was 1.73 on October 9, 2020 (the second wave) and 1.3 on March 17, 2021(the third wave). On the last day of the observation period, May 31, 2021, a decrease in the value of R to 0.46 was recorded. In this period, the Alpha variant (B.1.1.7) was dominant (97%), and the Delta variant (B.1.617.2) accounted for 2.28%. We found that 36.27% of the population received at least 1 dose of the vaccine during the study period [2].
Data characterizing the course of the pandemic in Poland during the study period in comparison with cumulative data from European Union countries are presented in Table 1.
There were 434.61 COVID-19 patients in hospital per million people in Poland on the start date of observation (November 1, 2020), the maximum value was 914.09 per 1 million population recorded on April 9, 2021, and it was 134.16 per 1 million population on the date of study completion of the observation, on May 31, 2021.
Understanding the factors affecting COVID-19 mortality and their ranking according to the importance of the impact on the effects of the COVID-19 pandemic seems to be crucial in public health decisions. There were 18.2 million cases excess deaths worldwide observed from January 1, 2020 to the end of December 2021. This is 3 times more than the number of registered deaths due to COVID-19 [3].
The highest numbers of excess deaths were observed in Latin America, Eastern Europe, and Central Europe. High rates were also recorded in countries with high economic status in the northern hemisphere. Relatively low mortality rates were observed in Australia and Asia-Pacific countries with high economic status [4].
Therefore, this retrospective study was conducted at a single center in Poland between November 2020 and May 2021 and aimed to evaluate the morbidity and mortality rates in 581 patients hospitalized with COVID-19.
Material and Methods
ETHICS:
This study was approved by the Bioethics Committee of the Medical University of Warsaw (AKBE/5/2023). It was based on data gathered during routine patient care and does not include any individual patient data.
PATIENTS:
This retrospective study was based on analysis of medical records of adult residents of central Poland who were admitted to a multi-specialty hospital temporarily transformed into an infectious disease hospital for the treatment of COVID-19, with symptoms of respiratory failure due to SARS-CoV-2 pneumonia from October 24, 2020 to May 31, 2021. The analyzed group consisted of 581 patients aged 19–99 years (average 69), including 229 women aged 48–99 years (average 73) and 352 men aged 31–95 years(average 66). There were 533 patients admitted from home, 21 patients transferred from other hospitals, and 27 from long-term care facilities.
THE SOURCE OF DATA:
The data were obtained from hospital electronic medical records containing results of subjective and objective examinations, laboratory tests, microbiological and imaging findings upon admission to the hospital and during hospitalization, and discharge summaries. In addition, the evaluation included the number of days from symptom onset to hospital admission, duration of hospitalization, comorbidities, and complications occurring during hospitalization. The observation period encompassed the entire hospitalization period due to severe COVID-19, concluding with discharge or patient death. Data analysis was conducted using Microsoft Excel for Microsoft 365.
SARS-COV-2 DIAGNOSTICS:
Diagnosis of COVID-19 was confirmed by commercial diagnostic tests for SARS-CoV-2 by quantitative reverse transcription polymerase chain reaction (RT-qPCR) detecting at least 2 different nucleocapsid gene regions (N1 and N2) of the virus that were validated and approved for use in the European Union in accordance with WHO recommendations [5].
SARS-CoV-2 RNA was detected from nasopharyngeal swabs, and from tracheal aspirates or bronchial lavage fluids in intubated patients. Diagnosis of COVID-19 pneumonia was confirmed by chest CT scan performed within 48 h of hospital admission, which showed changes typical of viral pneumonia (ground-glass opacities, crazy-paving pattern, consolidations) [6].
THE TREATMENT OF COVID-19:
The treatment of COVID-19 patients was in accordance with the current standards approved by the Ministry of Health of the Republic of Poland. The oxygen therapy included: passive oxygen therapy using a nasal catheter, a simple mask, a mask with a reservoir; high-flow nasal canula (HFNC); non-invasive methods of respiratory support: CPAP (continuous positive airway pressure), BIPAP (biphasic positive airway pressure); and mechanical ventilation. In case of persistent hypoxemia during passive oxygen therapy and HFNC, the prone position was used to improve oxygenation. The following drugs were used in pharmacotherapy were remdesivir, corticosteroids, tocilizumab, and low-molecular-weight heparin, in prophylactic and therapeutic doses, depending on indications [7].
ASSESSMENT OF MULTIMORBIDITY:
The CCI, which predicts survival of patients with multiple comorbidities, was used to assess multimorbidity [8]. The assessment was based on the sum of the scores obtained for comorbidities and the age of the patient [9,10]. Morbidity and mortality rates were determined as the percentage of occurrence in the total number of hospitalized patients, the percentage of occurrence in age groups, or the percentage of occurrence in males and females.
STATISTICS:
Statistical analysis was performed in the IBM SPSS Statistics program. The Pearson’s chi-squared test was used to determine statistically significant relationships between sex and age of patients and the occurrence of death, between sex and age of patients and the direct cause of death, and between individual comorbidities and death. The Kolmogorov-Smirnov test and the Kruskal-Wallis test were used to determine the correlation between multimorbidity based on CCI values and death. A statistically significant relationship between variables was considered to be a value of
Results
ALL HOSPITALIZED PATIENTS WITH COVID-19:
A group of 581 patients admitted with respiratory failure in the course of COVID-19 pneumonia was analyzed. Most (60%) were men, and 83% of all admitted patients were over 55 years of age. The largest group, about 30%, were patients aged 65 to 74, with a male predominance – about 20% of all admitted patients. Out of 581 admitted patients, 204 (35%) died, 357 (62%) were discharged, and 20 (3%) were transferred to other hospitals (Figure 1).
DECEASED PATIENTS WITH COVID:
Of the 204 patients who died, 86% were over the age of 65, and 61% were men. The largest number deaths among males was in the age group 65–84, and the most deaths among female was in those over 85 years of age. The percentage of hospital admission and hospital mortality in individual age groups by sex is presented in Table 2. Out of 229 admitted female patients, 79 died, which constituted 34.5% of all admitted female patients. Of the 352 admitted male patients, 125 died, which accounted for 35.5% of all admitted male patients. Patients transferred to another hospital were excluded from analysis. The mortality rate, excluding patients transferred to another hospital, was 36.4%.
RELATIONSHIP BETWEEN SEX AND AGE OF THE DECEASED:
To assess whether there was a relationship between sex and age of patients who died, the age categories up to 54 years of age were combined, because the numbers were too small to analyze separately. Mortality was similar in females (35.7%) and males (36.8%). The chi-square test showed no relationship between sex and mortality (chi-square=0.060,
The largest group of deceased female patients were those at least 85 years old (49.4%), and most deceased male patients were 65–74 years old (34.4%) and 75–84 years old (32%). In all age groups under 85, the mortality rate among males was is higher than among females. The chi-square test showed a significant relationship between sex and age of the deceased (chi-square=23.780,
NUMBER OF DAYS FROM SYMPTOM ONSET TO HOSPITAL ADMISSION:
All patients were admitted to the hospital 4–25 days after onset of COVID-19 symptoms. Deceased female patients had a shorter period between hospital admission and onset of COVID-19 symptoms than in the remaining groups of patients. Dominants (DO), median, and interquartile range (IQR) for hospital admission by sex are presented in Table 3.
THE RELATIONSHIP BETWEEN COMORBIDITIES AND DEATH:
The Kruskal-Wallis test showed that patients who died had a significantly higher CCI index than patients who survived and patients who were transferred to another hospitals (
Table 4 presents the proportions of deaths among individuals by individual comorbidities.
The diseases were listed from the highest to the lowest mortality rate. The chi-square test was calculated in such a way as to assess whether the percentage of deaths in patients with a given comorbidity was significantly higher than in patients who did not have a given disease. Thus, the chi-square test result proves that the percentage of deaths among patients with a given disease differs significantly from the percentage of deaths among patients without a given comorbidity, showing that the disease significantly increased the probability of death. Deaths were most common in patients with leukemia, all of which died, but there were only 4 patients with leukemia in the study group. Nevertheless, the chi-square test showed that despite the small group size, leukemia patients had a significantly higher risk of death from COVID-19.
We found that almost all analyzed comorbidities significantly increased the probability of death. The highest statistical significance strength (
DIRECT CAUSES OF DEATH:
Recorded direct causes of death in the study group were divided into 5 basic groups: COVID-19 lung disease, bacterial superinfections, thromboembolic complications and heart failure. COVID-19 lung disease includes deaths due to respiratory failure in the course of SARS-CoV-2 pneumonia, including pneumothorax.
Thromboembolic complications included pulmonary embolism, myocardial infarction, infarcts and embolisms located in other tissues, and ischemic stroke. Bacterial superinfections included VAP, hospital-acquired pneumonia (HAP), other sepsis-generalized infections with a source other than the respiratory system, neuroinfection, and pulmonary aspergillosis.
The relationship between sex and direct cause of death are presented in Table 5.
The chi-square test showed a statistically significant relationship between sex and the cause of death related to COVID-19 pneumonia and VAP. COVID-19 pneumonia was the direct cause of death in a significantly higher percentage of women (79.95%) than men (54.4%). VAP was the direct cause of death in a significantly higher proportion of men (21.6%) than women (6.3%). For other causes, no significant relationship with sex was found.
AGE AND CAUSE OF DEATH:
Age groups were compared in terms of causes of death. Due to the very small number of deceased patients below the age of 65, we created a single age group (25–64 years). The causes are listed in Table 6 from most common to least common.
The chi-square test showed significant differences between the age groups in terms of most of the common causes of death – COVID-19 lung disease, VAP, and other sepsis and thromboembolic complications.
COVID-19 lung disease was the cause of death much more often in patients aged 85 or more (80.3%) than in patients aged 26–64 (50%) or 65–74 (48.3%). Bacterial superinfections were the most common cause of death in patients aged 25–74. In particular, 14.3% of patients aged 25–64 died from sepsis with an origin other than pneumonia, but this caused no deaths in patients 85 years old or older. Other thrombotic-embolic complications were the cause of death almost exclusively among patients aged 75–84. No significant association with age was found for other causes.
Performing multiple comparisons of individual age groups, it can be concluded that:
Discussion
LIMITATIONS OF THE STUDY:
A limitation of our study was that the direct causes of death were determined on the basis of clinical data and were not confirmed by autopsy. In a few cases, more than 1 cause of death was specified.
One of questions we tried to answer was why did Poland have one of the highest COVID-19 mortality rates in Europe from November 2020 to May 2021, before the introduction of vaccination and effective treatment. A limitation of the study is that it was conducted as a retrospective single-center study and the results may not be generalizable nation-wide in Poland. For an objective analysis, it would be advisable to use data from at least a few hospitals from different regions of Poland and to include out-of-hospital deaths due to COVID-19 in the analysis.
Conclusions
This study shows that the women who died were significantly older than deceased men, but the mortality rates of male and female patients were similar. The most common direct cause of death in hospitalized COVID-19 patients was viral pneumonia, especially in patients over 85 years of age. The second most common cause was bacterial superinfection, which was more often the cause of death in younger patients. In addition, bacterial VAP as a cause of death was much more common in men than in women. The high COVID-19 mortality rate during the observation period may be related to the large number of elderly women in the general population of the country and the relatively high number of bacterial superinfections occurring as a complication of viral pneumonia. Currently, the introduction of protective vaccinations and appropriate treatment regimens has led to a very significant reduction in the mortality rate due to SARS-CoV-2.
Tables
Table 1. The most important epidemic indicators characterizing the course of the COVID-19 pandemic in Poland in from November 1, 2020 to May 31, 2021.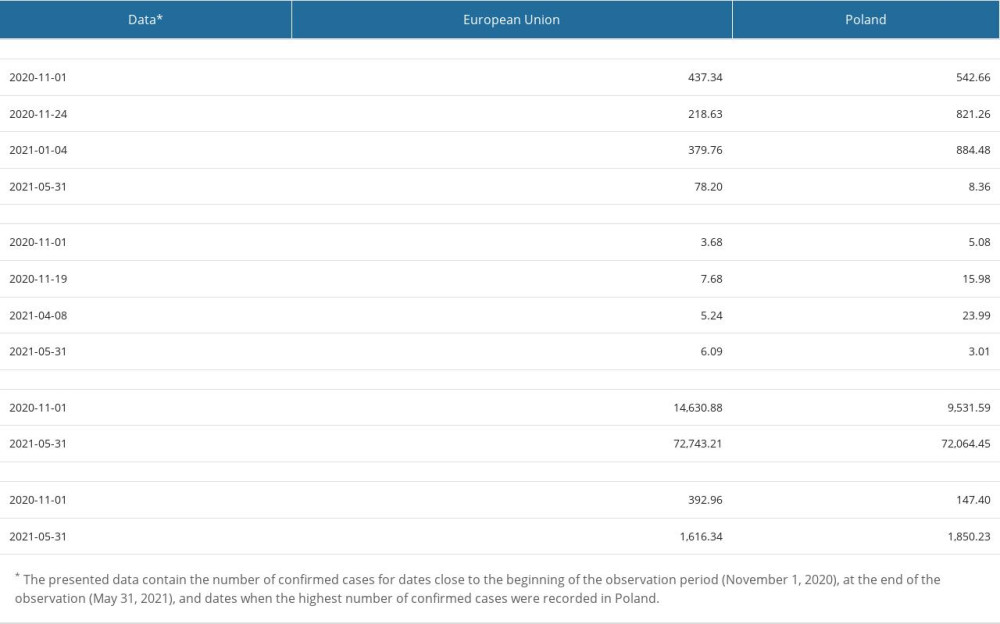 Table 2. Age groups of patients with COVID-19 admitted to hospital and in-hospital mortality.
Table 2. Age groups of patients with COVID-19 admitted to hospital and in-hospital mortality.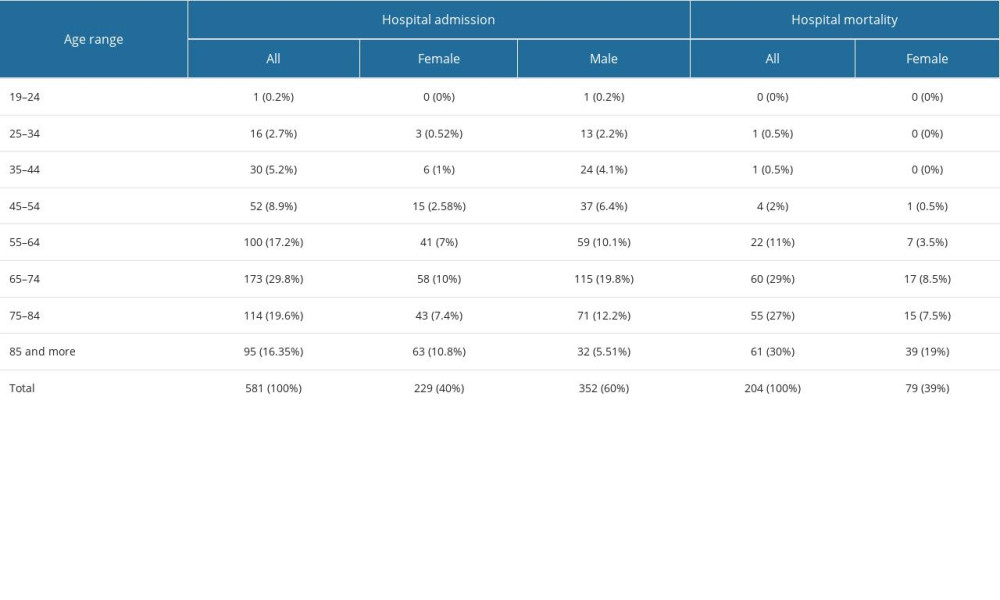 Table 3. Day of admission to the hospital from the onset of COVID-19 symptoms*.
Table 3. Day of admission to the hospital from the onset of COVID-19 symptoms*.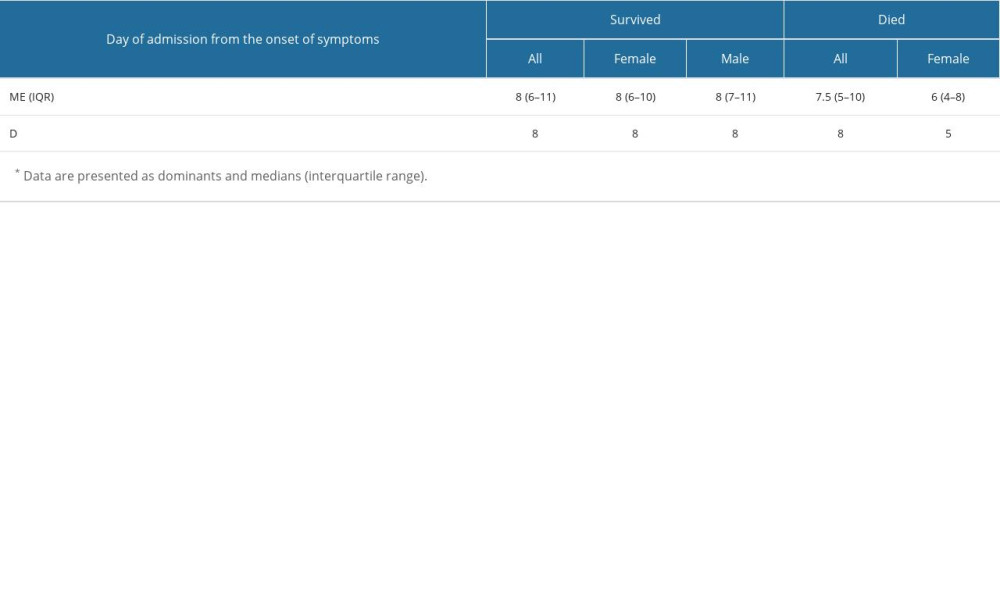 Table 4. The relationship between the incidence of individual comorbidities included in the Charles Comorbidity Index (CCI) and the occurrence of deaths in patients with COVID-19.
Table 4. The relationship between the incidence of individual comorbidities included in the Charles Comorbidity Index (CCI) and the occurrence of deaths in patients with COVID-19.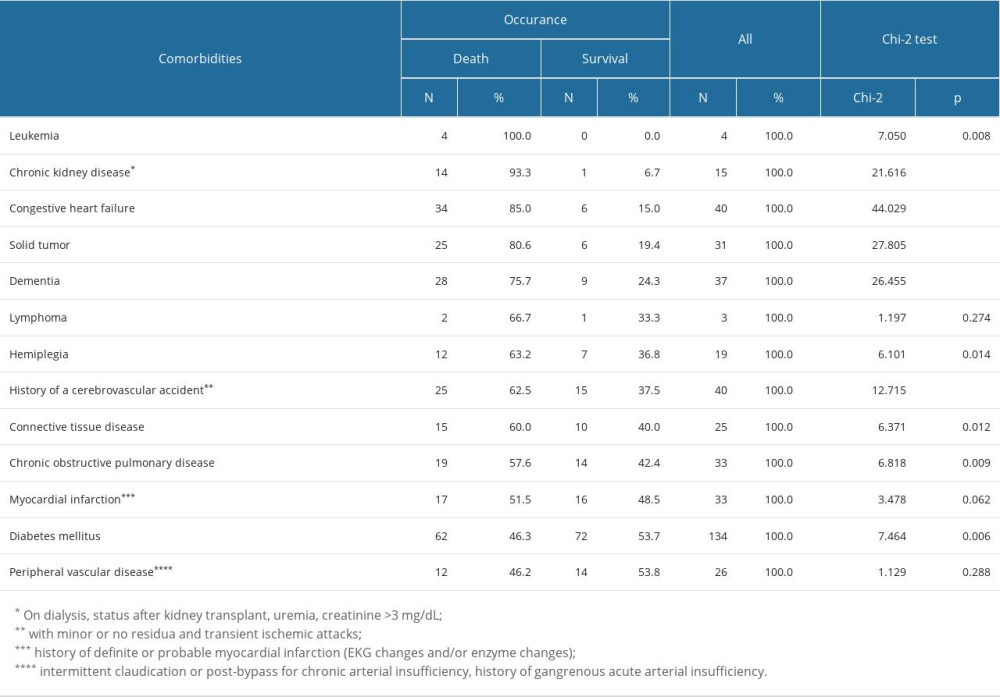 Table 5. Relationship between sex and direct cause of death in patients with COVID-19*.
Table 5. Relationship between sex and direct cause of death in patients with COVID-19*.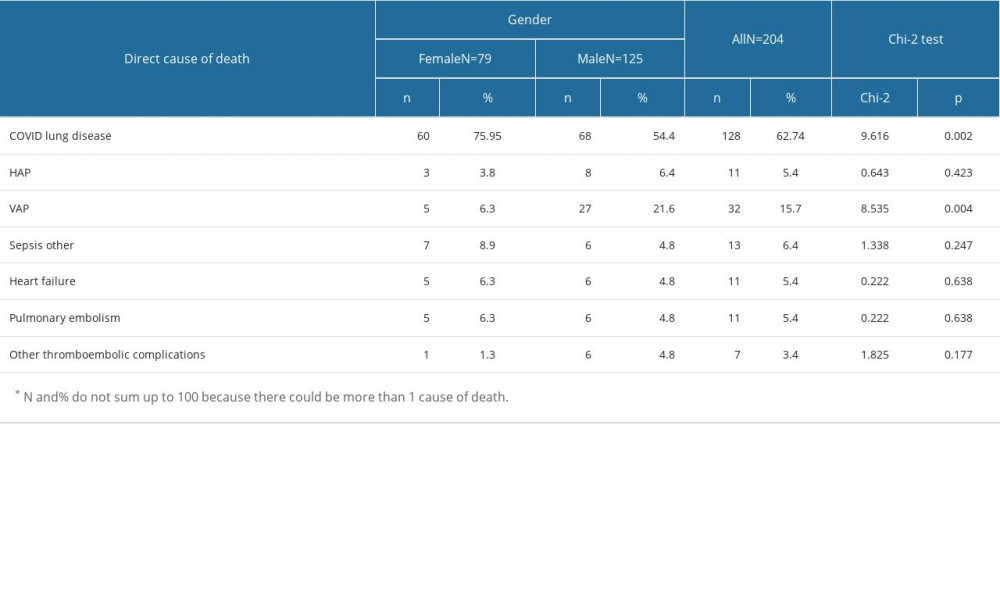 Table 6. Relationship between age and cause of death in patients with COVID-19*.
Table 6. Relationship between age and cause of death in patients with COVID-19*.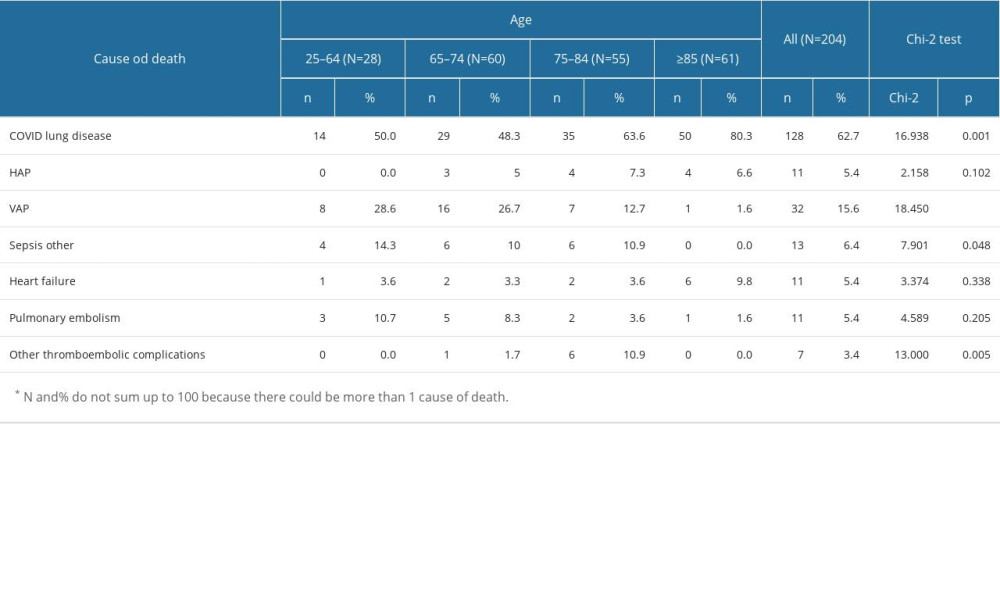
References
1. : The World Factbook, Central Intelligence Agency https://www.cia.gov/the-world-factbook/countries/poland/
2. Our World in Data: Coronavirus (COVID-19) Data Explorer https://ourworldindata.org/coronavirus/poland/
3. : The true death toll of COVID-19: estimating global excess mortality , World Health Organization https://www.who.int/data/stories/the-true-death-toll-of-COVID-19-19-estimating-global-excess-mortality
4. COVID-19 Excess Mortality Collaborators, Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–21 [published correction appears in Lancet. 2022;399(10334):1468]: Lancet, 2022; 399(10334); 1513-36
5. Premraj A, Aleyas AG, Nautiyal B, Rasool TJ, Nucleic acid and immunological diagnostics for SARS-CoV-2: Processes, platforms and pitfalls: Diagnostics (Basel), 2020; 10(11); 866
6. Simpson S, Kay FU, Abbara S, Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA – secondary publication: J Thorac Imaging, 2020; 35(4); 219-27
7. Flisiak R, Zarębska-Michaluk D, Knowledge is coming so fast that a meta-analysis of COVID-19 treatment is always too late: Pol Arch Intern Med, 2020; 130(9); 721-23
8. MDCalc: Charlson Comorbidity Index (CCI) https://www.mdcalc.com/charlson-comorbidity-index-cci
9. Tuty Kuswardhani RA, Henrina J, Pranata R, Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis: Diabetes Metab Syndr, 2020; 14(6); 2103-109
10. Elo IT, Luck A, Stokes AC, Evaluation of age patterns of COVID-19 mortality by race and ethnicity from March 2020 to October 2021 in the US [published correction appears in JAMA Netw Open. 2022;5(8):e2228383]: JAMA Netw Open, 2022; 5(5); e2212686
11. Dessie ZG, Zewotir T, Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients: BMC Infect Dis, 2021; 21(1); 855
12. Leidi F, Boari GEM, Scarano O, Comparison of the characteristics, morbidity and mortality of COVID-19 between first and second/third wave in a hospital setting in Lombardy: A retrospective cohort study: Intern Emerg Med, 2022; 17(7); 1941-49
13. Giacomelli A, Ridolfo AL, Milazzo L, 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: A prospective cohort study: Pharmacol Res, 2020; 158; 104931
14. Nada KM, Hsu ES, Seashore J, Determining cause of death during coronavirus disease 2019 pandemic: Crit Care Explor, 2021; 3(4); e0419
15. Levin AT, Hanage WP, Owusu-Boaitey N, Assessing the age specificity of infection fatality rates for COVID-19: Systematic review, meta-analysis, and public policy implications: Eur J Epidemiol, 2020; 35(12); 1123-38
16. Zhou F, Yu T, Du R, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study [published correction appears in Lancet. 2020;395(10229):1038]: Lancet, 2020; 395(10229); 1054-62
17. Gupta S, Hayek SS, Wang W, Factors associated with death in critically ill patients with coronavirus disease 2019 in the US [published correction appears in JAMA Intern Med. 2021;181(8):1144; JAMA Intern Med. 2020;180(11): 1555]: JAMA Intern Med, 2020; 180(11); 1436-47
18. Imam Z, Odish F, Gill I, Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States: J Intern Med, 2020; 288(4); 469-76
19. Cisterna-García A, Guillén-Teruel A, Caracena M, A predictive model for hospitalization and survival to COVID-19 in a retrospective population-based study: Sci Rep, 2022; 12(1); 18126
20. Li Q, Zhao C, A Review of the current status of clinical management of COVID-19 in the elderly: Med Sci Monit, 2021; 27; e930278
21. Elezkurtaj S, Greuel S, Ihlow J, Causes of death and comorbidities in hospitalized patients with COVID-19: Sci Rep, 2021; 11(1); 4263
22. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators, Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: A prospective cohort study: Intensive Care Med, 2021; 47(1); 60-73
23. : WHO Therapeutics and COVID-19: Living guideline https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2022.4
24. Rahmani K, Shavaleh R, Forouhi M, The effectiveness of COVID-19 vaccines in reducing the incidence, hospitalization, and mortality from COVID-19: A systematic review and meta-analysis: Front Public Health, 2022; 10; 873596
25. Nab L, Parker EPK, Andrews CD, Changes in COVID-19-related mortality across key demographic and clinical subgroups in England from 2020 to 2022: A retrospective cohort study using the OpenSAFELY platform: Lancet Public Health, 2023; 8(5); e364-e77
26. Tenforde MW, Link-Gelles R, Reduction in COVID-19-related mortality over time but disparities across population subgroups: Lancet Public Health, 2023; 8(5); e327-e28
27. Baker TB, Bolt DM, Smith SS, The relationship of COVID-19 vaccination with mortality among 86,732 hospitalized patients: Subpopulations, patient factors, and changes over time: J Gen Intern Med, 2023; 38(5); 1248-55
Tables
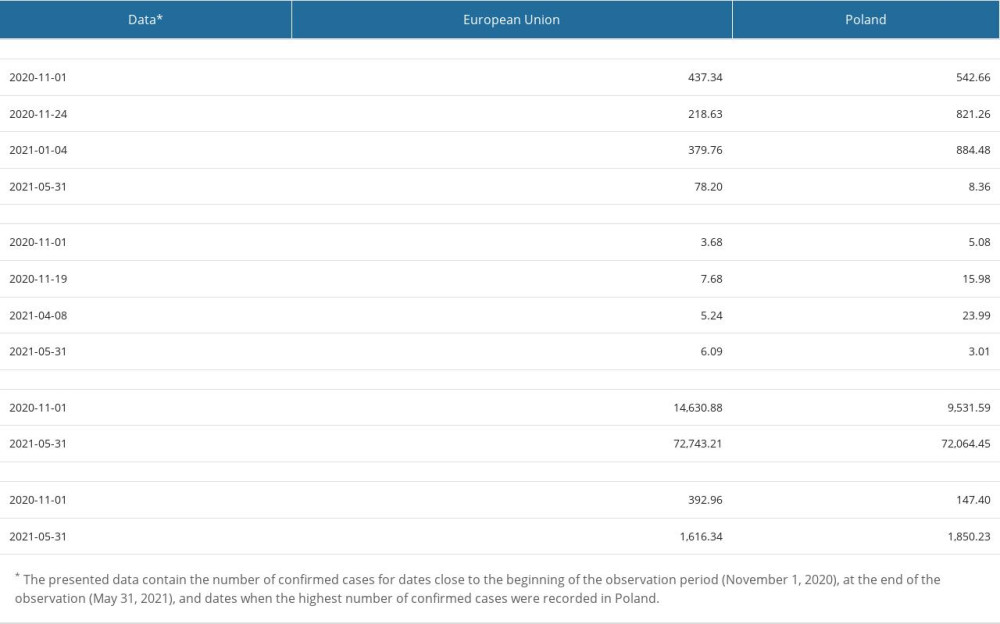 Table 1. The most important epidemic indicators characterizing the course of the COVID-19 pandemic in Poland in from November 1, 2020 to May 31, 2021.
Table 1. The most important epidemic indicators characterizing the course of the COVID-19 pandemic in Poland in from November 1, 2020 to May 31, 2021.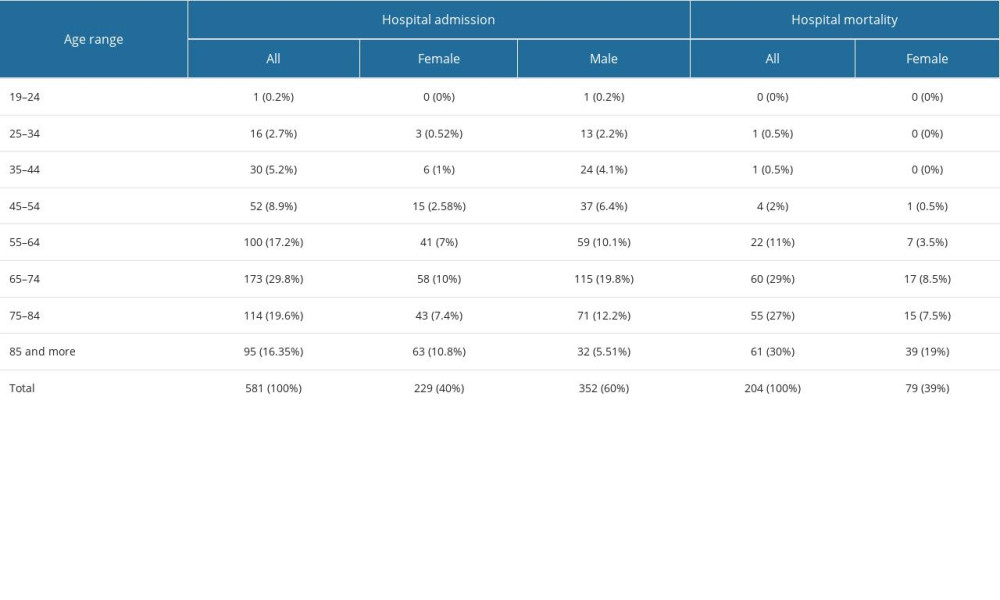 Table 2. Age groups of patients with COVID-19 admitted to hospital and in-hospital mortality.
Table 2. Age groups of patients with COVID-19 admitted to hospital and in-hospital mortality.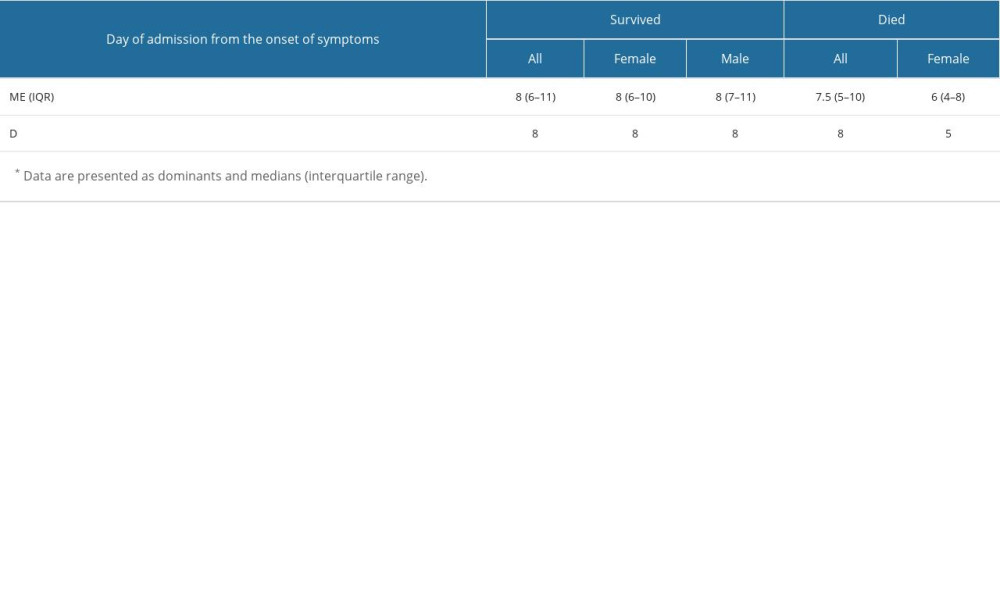 Table 3. Day of admission to the hospital from the onset of COVID-19 symptoms*.
Table 3. Day of admission to the hospital from the onset of COVID-19 symptoms*.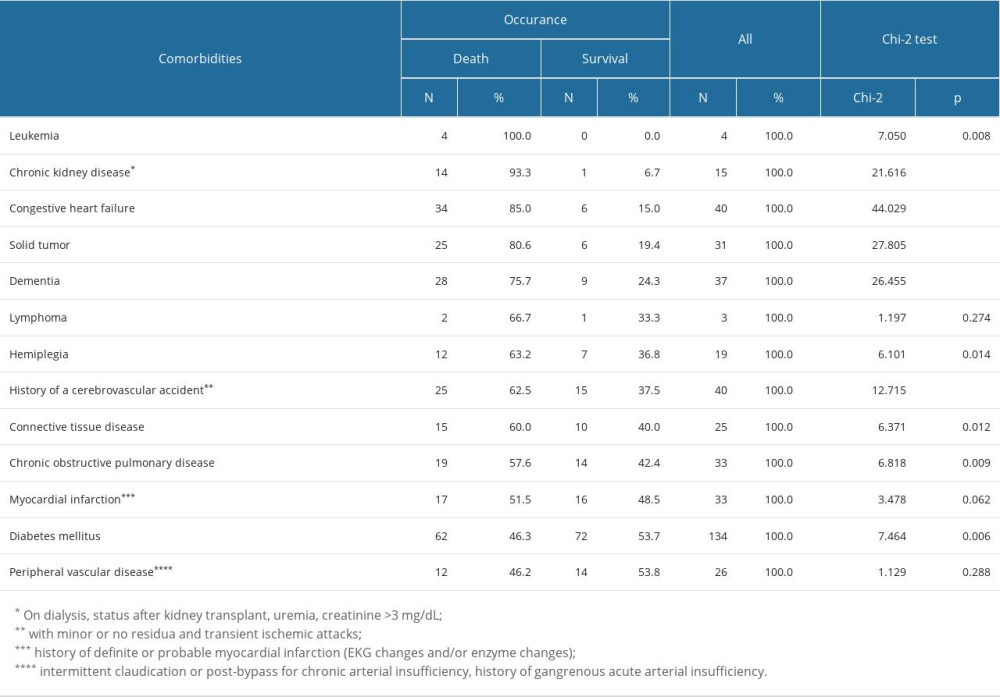 Table 4. The relationship between the incidence of individual comorbidities included in the Charles Comorbidity Index (CCI) and the occurrence of deaths in patients with COVID-19.
Table 4. The relationship between the incidence of individual comorbidities included in the Charles Comorbidity Index (CCI) and the occurrence of deaths in patients with COVID-19.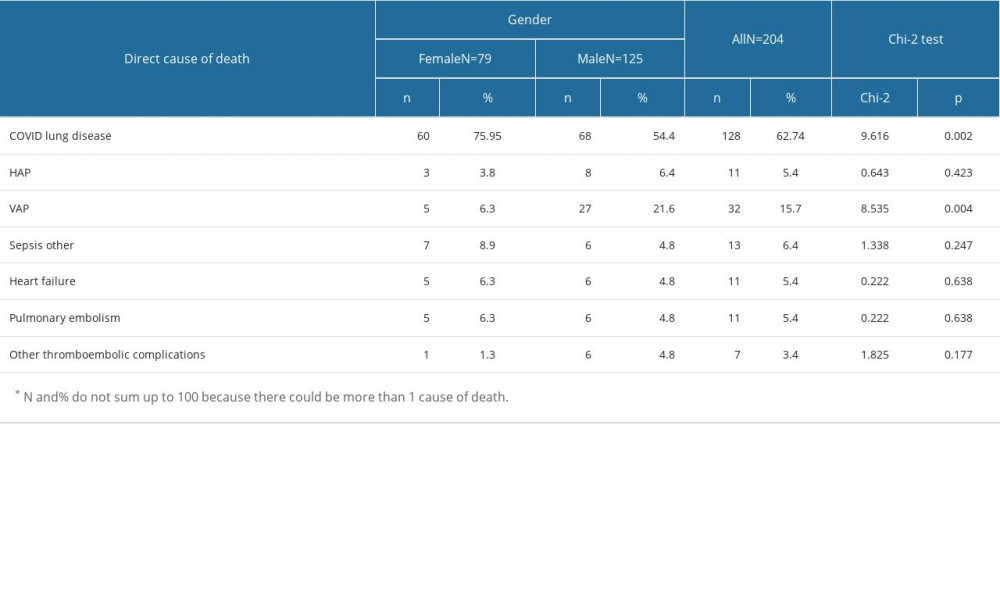 Table 5. Relationship between sex and direct cause of death in patients with COVID-19*.
Table 5. Relationship between sex and direct cause of death in patients with COVID-19*.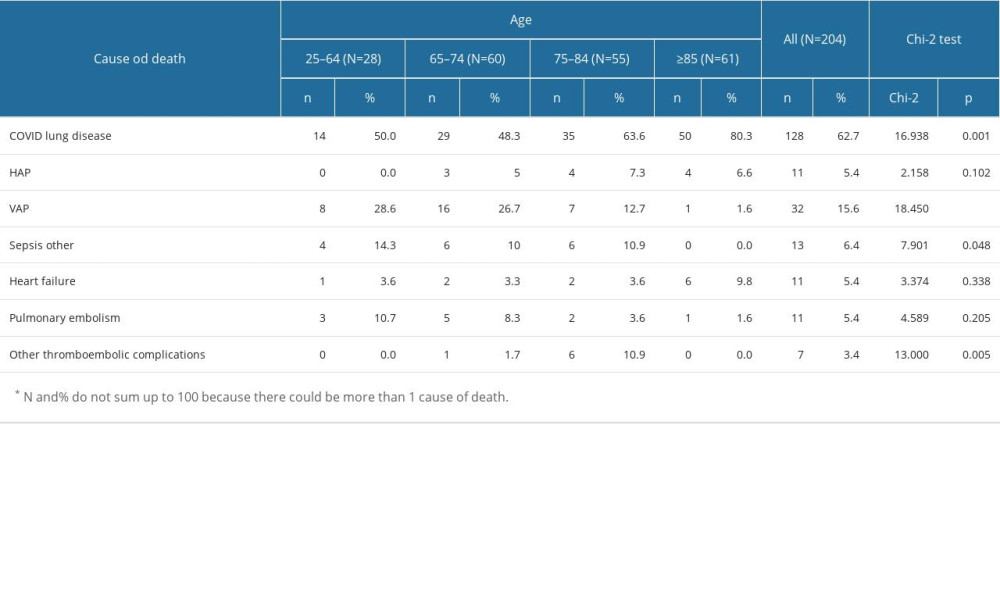 Table 6. Relationship between age and cause of death in patients with COVID-19*.
Table 6. Relationship between age and cause of death in patients with COVID-19*.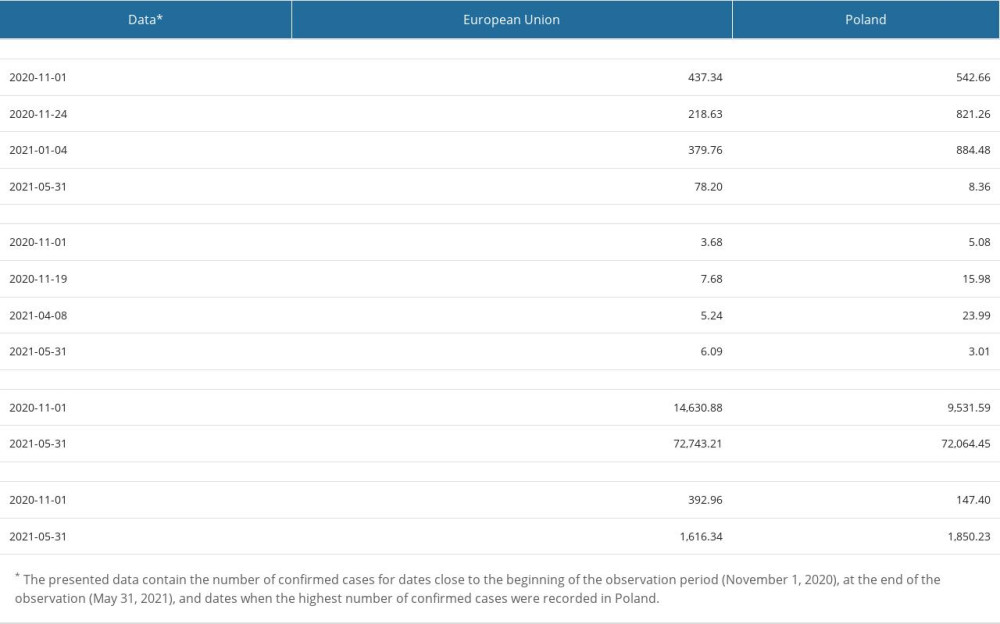 Table 1. The most important epidemic indicators characterizing the course of the COVID-19 pandemic in Poland in from November 1, 2020 to May 31, 2021.
Table 1. The most important epidemic indicators characterizing the course of the COVID-19 pandemic in Poland in from November 1, 2020 to May 31, 2021.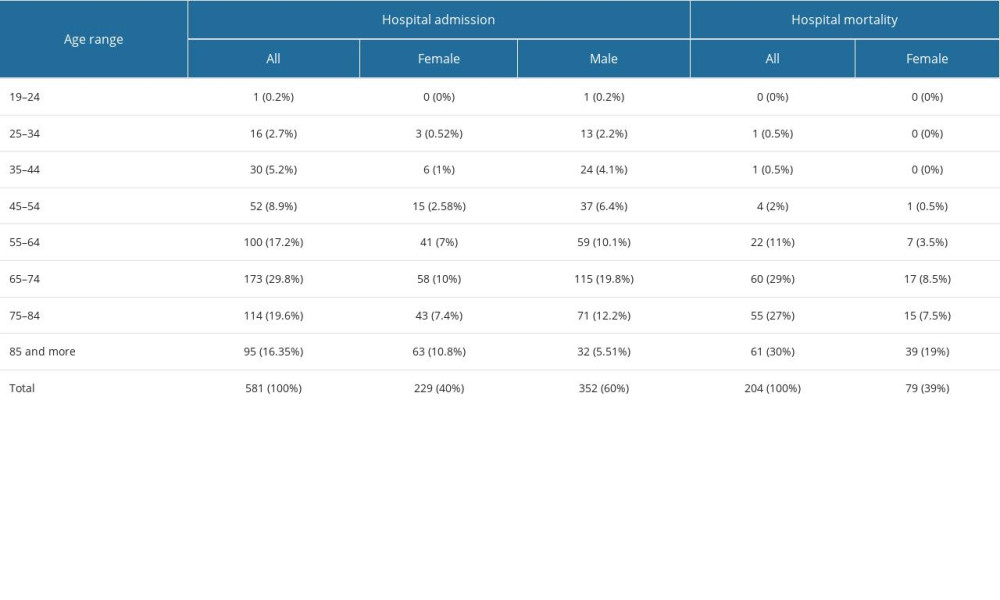 Table 2. Age groups of patients with COVID-19 admitted to hospital and in-hospital mortality.
Table 2. Age groups of patients with COVID-19 admitted to hospital and in-hospital mortality.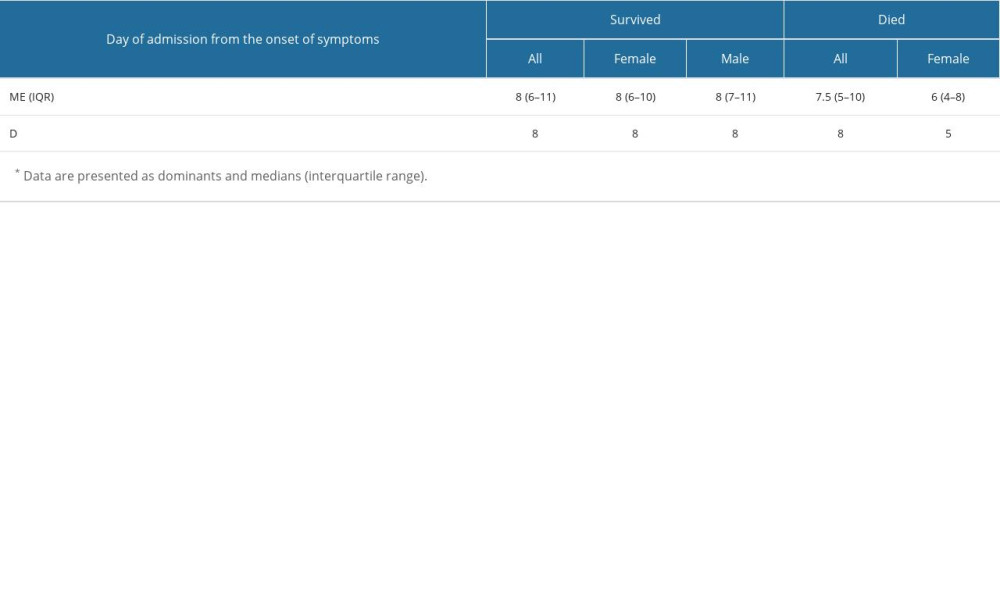 Table 3. Day of admission to the hospital from the onset of COVID-19 symptoms*.
Table 3. Day of admission to the hospital from the onset of COVID-19 symptoms*.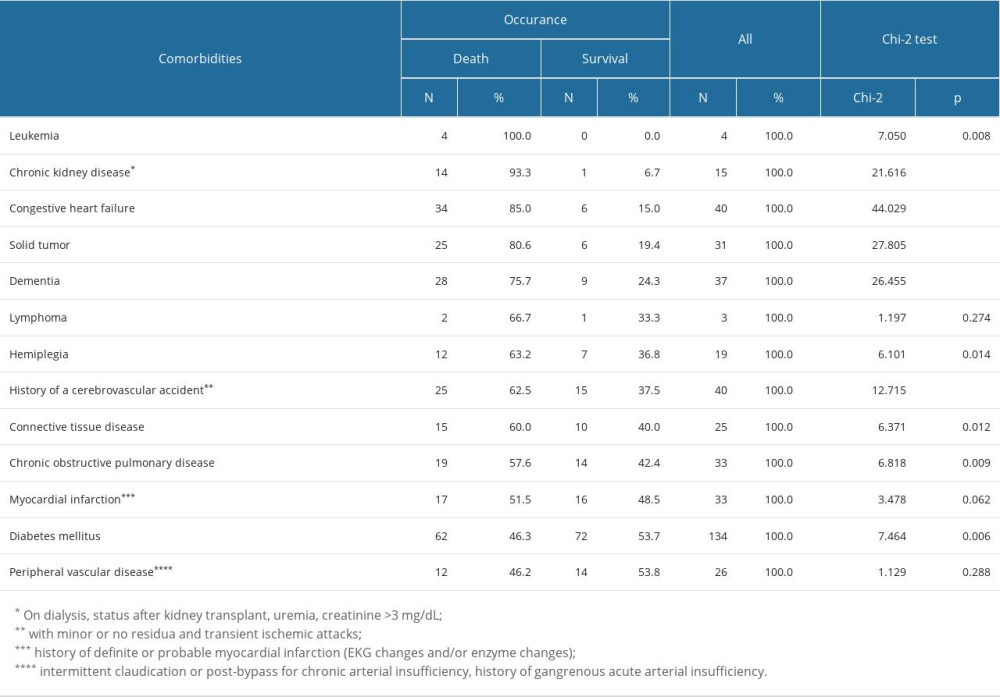 Table 4. The relationship between the incidence of individual comorbidities included in the Charles Comorbidity Index (CCI) and the occurrence of deaths in patients with COVID-19.
Table 4. The relationship between the incidence of individual comorbidities included in the Charles Comorbidity Index (CCI) and the occurrence of deaths in patients with COVID-19.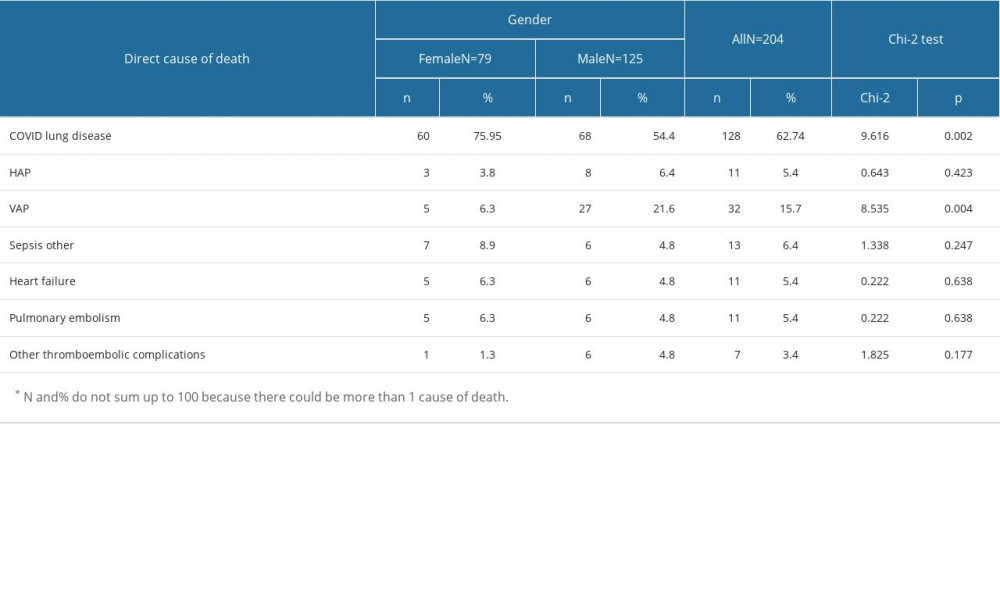 Table 5. Relationship between sex and direct cause of death in patients with COVID-19*.
Table 5. Relationship between sex and direct cause of death in patients with COVID-19*.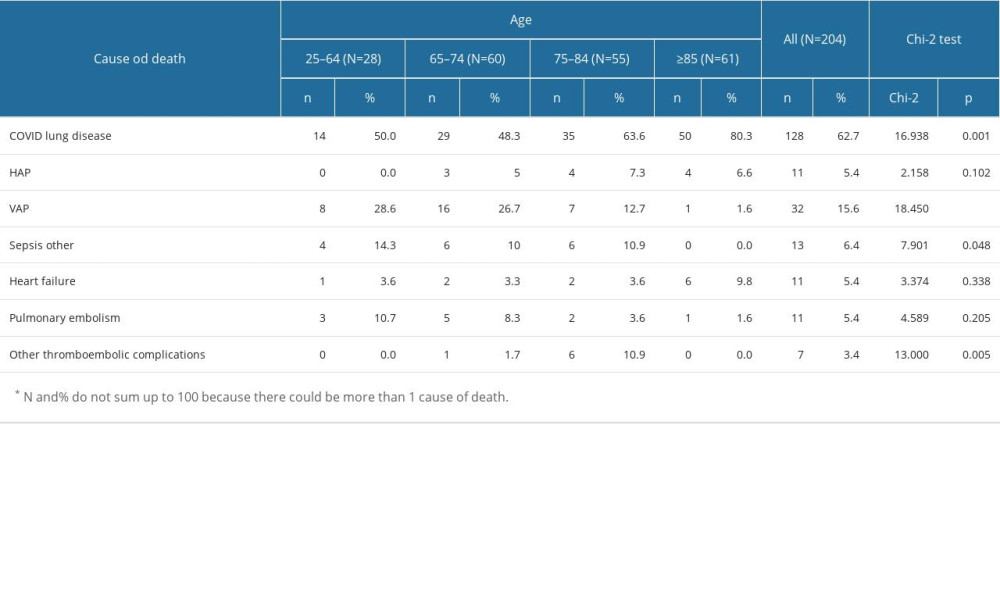 Table 6. Relationship between age and cause of death in patients with COVID-19*.
Table 6. Relationship between age and cause of death in patients with COVID-19*. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952