22 January 2024: Clinical Research
Comparative Outcomes of Early, Elective, and Delayed Treatment for Lateral Condyle Fracture of the Humerus in Children: A Retrospective Study from a Single Center in Turkey (2013–2021)
Sait Anıl UlusDOI: 10.12659/MSM.942728
Med Sci Monit 2024; 30:e942728
Abstract
BACKGROUND: Lateral condyle fracture of the humerus in children should be diagnosed and treated quickly to avoid the complications of malunion and varus deformity of the elbow. Worldwide, pediatric orthopedic departments experienced delays in patient diagnosis and treatment during the COVID-19 pandemic. This retrospective study from a single center in Turkey aimed to compare outcomes from early treatment, elective treatment, and delayed treatment in 140 children with lateral condyle fracture of the humerus between 2013 and 2021.
MATERIAL AND METHODS: In the study, 140 patients with Milch type 2 fractures were included. Patients underwent fixation with K-wires or screws after open or closed reduction. Data collected included age, sex, trauma details, surgery timing, operating conditions, perioperative issues, and rehabilitation outcomes. Fracture union and complications were monitored through clinical examinations and X-rays. Clinical outcomes were evaluated using the Mayo Elbow Performance Score (MEPS).
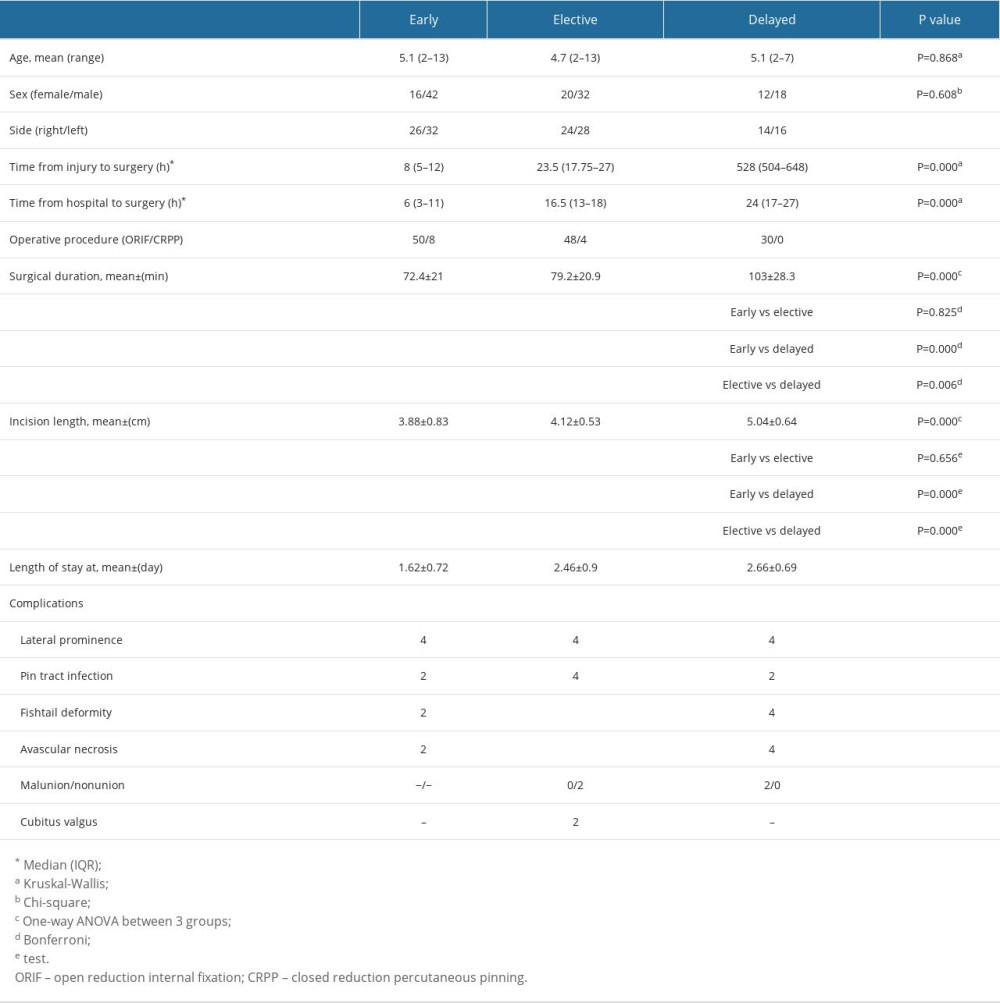
RESULTS: There were 58 patients in the early group, 52 in the elective group, and 30 in the delayed group. Surgery durations varied among the groups (P=0.000). The early and delayed groups as well as the early and elective groups had significantly different incision sizes (P=0.000 for both). The early and delayed groups and the early and elective groups had significantly different MEPS scores (P=0.002 and P=0.011, respectively).
CONCLUSIONS: In patients with late-presenting lateral condyle fractures, although complications increase, surgical treatment does not yield worse outcomes. Standardization of fracture management should be maintained during periods such as COVID-19.
Keywords: COVID-19, humeral fractures, delayed diagnosis
Background
The second most frequent elbow fracture in children is a fracture of the humeral lateral condyle, which accounts for 12% to 20% of all fractures of the upper extremities in children. [1]. Children between the ages of 4 and 10 years are most likely to sustain one of these fractures, with children 6 years old having the highest prevalence. The most frequently described mechanism is a fall onto an extended hand when the elbow is extended and the forearm is supinated (pull-off mechanism) [2]. Other injury mechanisms include direct trauma to the elbow and valgus impaction at the elbow that fractures the lateral condyle (push-off mechanism) [3]. Ecchymosis and elbow discomfort are signs of a fracture on physical examination. The majority of the time, plain radiographs are used to identify lateral condyle fractures. Radiographs of the elbow’s anteroposterior, internal oblique, and lateral positions must be taken [4]. Young children’s distal humeri are cartilaginous, which makes them difficult to see on plain radiographs. An arthrogram can be used to either aid in intraoperative fracture reduction of the articular surface or to help define characteristics of the fracture for a more accurate diagnosis [5]. When results from conventional radiographs are unclear, magnetic resonance imaging and ultrasonography can be used to evaluate the integrity of the cartilage surface in minimally displaced lateral condyle fractures [6]. If the displacement between fractured fragments is less than 2 mm, conservative treatment is generally recommended [7]. A long arm cast is applied with the elbow positioned at 90° of flexion and the forearm positioned in neutral rotation [8]. There is little controversy that fragment displacement >2 mm and an incongruent articular surface are the primary indications for surgery. Surgical management includes both closed reduction with fixation and open reduction and internal fixation (ORIF) as options [9]. In patients presenting late, ORIF can be performed. Additionally, corrective osteotomies for cubitus valgus or varus, ulnar nerve transposition, and pseudoarthrosis surgery are sometimes applied [10].
Although the lateral condyle fracture of the humerus is one of the most frequent pediatric elbow injuries [10], there are still questions about how to manage acute, ignored, or even delayed-presented fractures. In cases in which the diagnosis of these fractures is delayed, complications such as painful and restricted joint movements, cubitus valgus deformity, and consequent ulnar nerve neuropathy, elbow instability, and growth arrest at the distal humerus physis can occur. When treated late, complications such as reduced range of joint motion, avascular necrosis of the fragment, and infection can be observed [11]. Early surgical intervention for lateral condyle fracture of the humerus may be able to avoid issues including infection, malunion, and nonunion [12]. Numerous publications have noted that reducing the condyle to its anatomical position becomes increasingly challenging the longer lateral condyle fracture of the humerus is left untreated. This is likely to make things more complicated and have an impact on the outcome [13]. Albeit, surgery is strongly recommended for patients who arrive late [14].
Not many studies have compared early and delayed surgery for displaced lateral condyle fractures of the humerus [10,15]. Pediatric lateral condyle fractures can require emergency care or can wait for elective procedures. Children who arrive mostly during the daytime should be operated on by the operating room team on duty at night if it is deemed an emergency. Operations carried out at night are more complicated [16]. Additionally, cultural practices, such as the use of bonesetters in developing nations and global health crises like the COVID-19 pandemic, might prolong and complicate the identification and care of these fractures [17]. Therefore, this retrospective study from a single center in Turkey aimed to compare outcomes from early treatment, elective treatment, and delayed treatment in 140 children with lateral condyle fracture of the humerus between 2013 and 2021.
Material and Methods
ETHICAL STATEMENT:
This study was approved by the Ethics Review Committee of Dicle University (approval number: 268-2023). The study was conducted following the ethical principles of the Declaration of Helsinki, and the participants or their families provided written informed consent.
PARTICIPANTS AND DESIGN:
Our hospital database identified 140 pediatric patients with lateral condyle fractures of the humerus from March 2013 to September 2021. Patients who underwent surgery within 0 to 12 h were called early (n=58); 12 to 48 h, elective (n=52); and 3 to 12 weeks, delayed (n=30). Patients who had surgery the same day were in the early group. Elective patients underwent surgery the day after presentation due to anesthetic issues, hunger, COVID-19-related operating room problems, or pediatric consultations. The delayed group consisted of latecomers. Most patients in the delayed group consisted of individuals who did not seek early treatment during the periods of lockdown that were imposed because of to COVID-19. Creating early and elective groups evaluated how timing affects pediatric lateral condyle fracture outcomes.
INCLUSION AND EXCLUSION CRITERIA:
Inclusion criteria were patients aged 2 to 14 years with unilaterally closed Milch type II fractures who underwent closed reduction percutaneous pinning or ORIF surgery, had a fracture displacement more than 2 mm, and had a follow-up of at least 1 year. Exclusion criteria were patients with Milch type I fractures, open fractures, pathological fractures, combination fractures affecting target elbow joint rehabilitation, operation between 48 h and 3 weeks, compartment syndrome, substantial neurovascular insufficiency, and lack of follow-up data.
SURGICAL TECHNIQUE:
Under fluoroscopy, closed reduction maneuvers were performed on the operating side. Patients with delayed fractures or who failed to reduce after 2 or 3 attempts had open reduction. To accomplish an open reduction, a lateral elbow joint incision of 4 to 5 cm was done under general anesthesia. An open reduction was performed after scar tissue removal from the fracture site. After direct confirmation of anatomical reduction, several 1.5-mm or 2.0-mm Kirschner wires (K-wires) or screws were implanted from the lateral condyle under careful articular surface inspection. The posterior lateral condylar fragment’s soft tissue attachment was protected during surgery. Pin and wire arrangements were fluoroscopically confirmed. K-wires were unburied and covered with iodoform gauze. A useful long arm cast immobilized the arm for 4 to 6 weeks after surgery. In Figure 1, an 8-year-old male patient presenting with a non-displaced fracture from the early group is shown. In Figure 2, a 7-year-old female patient from the delayed group is shown.
POSTOPERATIVE CARE AND FOLLOW-UP:
Clinical and radiographic evaluations were scheduled every 2 weeks after surgery until bone union was confirmed. The cast and K-wires were removed in the outpatient clinic if an X-ray 4 to 6 weeks following surgery showed a callus over the fracture gap. Functional rehabilitation exercises began.
DATA COLLECTION:
The results were analyzed for patients with only Milch type 2 fractures who underwent open or closed reduction followed by fixation with K-wire or screws. Age, sex, trauma type, side, time from injury to surgery, time from hospital to surgery, operation duration, incision size, perioperative problems, and functional rehabilitation outcomes were among the data gathered from the patients. Subtle infections, nonunions, malunions, lateral condylar prominence, cubitus valgus deformity, fishtail deformity, and osteonecrosis of the lateral humeral condyle were among the complications that were noted.
INDICATORS OF TREATMENT RESULTS:
At the most recent follow-up, the Baumann angle and the carrying angle of the injured limb were measured in each of the 3 groups. The following measurements were made for functional scores:
The Mayo Elbow Performance Score (MEPS) [18] was used to assess elbow joint function at the final follow-up, which included pain (45 points), elbow stability (10 points), range of motion (20 points), and daily functional tasks (25 points). Higher scores out of 100 indicated better elbow function, and scores were categorized as excellent (90–100), good (75–89), fair (60–74), and poor (0–59).
STATISTICAL ANALYSIS:
The mean and standard deviation represented continuous data. The
LEVEL OF EVIDENCE:
This was a level III, retrospective comparative study.
Results
PATIENT DEMOGRAPHICS:
The mean age was determined to be 5 years (range, 2–13 years) among the 140 cases investigated, with 92 boys (66%) and 48 girls (34%). The mean age and sex distribution of the groups are shown in Table 1. Age and sex did not significantly differ between the groups (P=0.868 and P=0.608, respectively). Among the patients, 98 (70%) had a simple fall injury; 24 (17%), playground injury; 10 (7.1%), a sports injury; and 8 (5.7%), a height fall injury. There were more delayed incidents (13/30) in 2020 and 2021, while the nation was under a COVID-19 curfew (Figure 3).
PERIOPERATIVE PARAMETERS:
The median interval from injury to surgery in the early group was 8 h (interquartile range [IQR]: 5–12), in the elective group it was 23.5 h (IQR: 17.75–27), and in the delayed group it was 528 h (IQR: 504–648) (
Analysis of patient surgery durations showed the early group had a mean of 72.4±21 min, the elective group had 79.2±20.9 min, and the delayed group had 103±28.3 min. The surgery duration differed between groups (
We examined patients’ surgical incision lengths. The early group had a mean incision length of 3.88±0.83 cm, the elective group of 4.12±0.53 cm, and the delayed group of 5.04±0.64 cm. The groups differed greatly. The early and elective groups had similar incision sizes (
In 114 patients, 2 K-wires were used during surgery. At least 26 patients needed a third K-wire or compression screw implant. In terms of additional implants required, the early and elective groups were not different (
The hospital stay duration was 1.62 ±0.72 days for early patients, 2.46±0.90 days for elective patients, and 2.66±0.69 days for delayed patients. There was a significant difference between the early and elective groups and between early and delayed groups (
COMPLICATIONS:
Of the 140 patients, 34 (24%) had complications. The number of complications and details of the groups are given in Table 1. In terms of complications, there was no statistically significant difference between the groups (P=0.20; Table 1).
TREATMENT OUTCOMES:
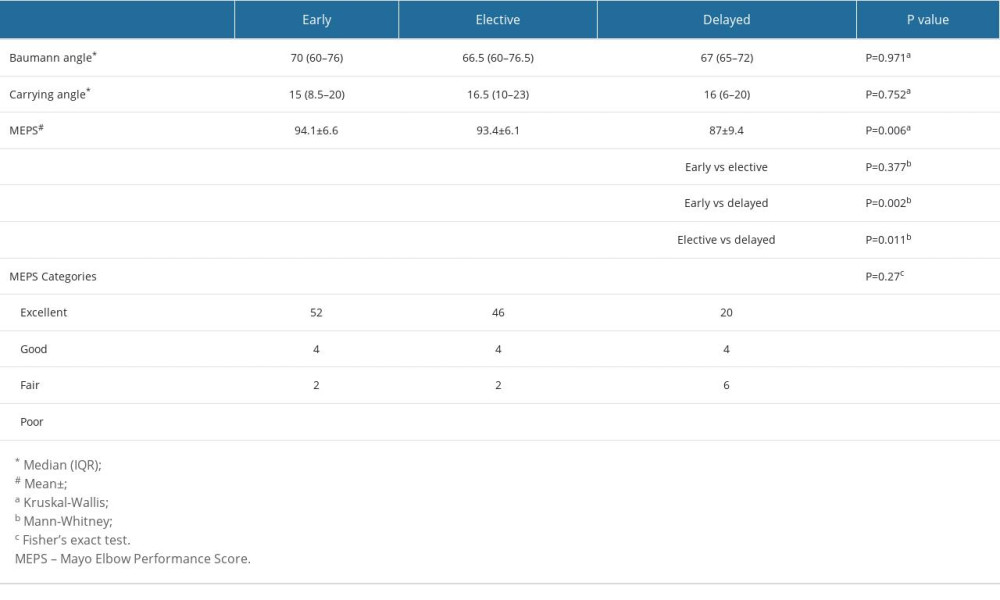
Baumann and carrying angles and MEPS values of the groups are given in Table 2. Between the groups, there were no discernible differences in carrying angle or Baumann (P=0.971 and P=0.752, respectively). Between the early and elective groups, the MEPS did not differ (P=0.377). The early and delayed groups as well as the elective and delayed groups differed significantly (P=0.002 and P=0.011, respectively).
According to the MEPS classification, no significant differences were observed between the groups (
Time from injury to surgery and patients’ MEPS were found to be negatively correlated (P=0.000, r=−0.414). A positive correlation was found between time from injury and operation time (P=0.001 r=0.383). A positive correlation was found between time from injury and incision length (P=0.000 r=0.543; Table 2).
Discussion
In this study, preoperative, intraoperative, and postoperative parameters of 140 patients treated at 3 time intervals were examined. More delayed incidents occurred during the COVID-19 curfew in 2020 and 2021. It was observed that in patients who presented later, the surgical duration was longer, the incision length was greater, and complications were more frequent. Additionally, these patients had a longer hospital stay compared with that of others. The early treatment group had higher MEPS than the delayed treatment group. We categorized patients into 3 groups based on their time to undergo surgery. We not only examined the results of early and delayed treatments but also investigated whether there were any changes in outcomes when minor delays occurred for various reasons in patients who presented early. In this regard, we are presenting what we believe to be the first study of its kind in the literature.
The age distribution, sex distribution, and types of trauma of the patients in our study are similar to that of studies in the literature [13,19,20]. Reasons for delayed surgery in the elective group compared with the early group include anesthesia not being deemed appropriate, unavailability of the operating room, pediatric consultations, and patients presenting at night. In the delayed group, the duration after the presentation was also longer. The reasons for this included swelling, skin wounds, and the time required to manage complications from incorrect treatments administered by non-medical practitioners. Additionally, 32% of patients sought medical attention during the pandemic, making the operating room unavailable at all times. Consequently, during the lockdown period of the pandemic, patients sought treatment from traditional bonesetters and experienced delays in seeking hospital care [21]. These delays and incorrect treatments hindered their ability to undergo early surgery upon eventual presentation [22,23]. However, the delay observed in the delayed group cannot be solely attributed to the pandemic. In developing countries, it is a reality that children are often taken to bonesetters by their parents, and various excuses are provided [24]. Indeed, when obtaining medical histories from the delayed group, they often cited reasons such as not wanting to visit hospitals due to the pandemic and fearing the outbreak. The high number of total admissions (32% of all patients) during the peak period of the pandemic in 2020–2021 further complicated the management of these fractures. This was because, during the period of intense restrictions, more patients were directed to our center due to the possibility of a COVID-19 diagnosis. In the study conducted by Muhammad et al, it was reported that during the pandemic period, there were delays in the treatment of pediatric patients. Patients arriving at the hospital were operated on later due to limited operating rooms, and the time between hospital admission and receiving treatment was longer than in the pre-pandemic period [21].
In a study conducted by James et al, 268 patients were examined [7]. They applied conservative treatment to 90.7% of patients at the initial presentation. Subsequently, 72 patients required surgery due to displacement during follow-ups, resulting in a total of 36.2% of patients undergoing surgery. In our study, all patients underwent surgery. Initially, our surgical percentage might appear high. This is because all patients had Milch type 2 fractures, and the majority presented with displaced fractures. In contrast, in the study by James et al, 51.5% of patients presented with non-displaced fractures, and the study included both Milch type 1 and type 2 fractures.
The early group spent much less time in the hospital than the other groups. However, since the patients’ postoperative hospital stays cannot be thoroughly assessed, no definitive conclusions can be made concerning the postoperative period. This could be considered a weakness of the study.
All of the patients in the delayed group presented 3 weeks after the injury. As in prior researches [14,15], every one of these individuals needed an open reduction. These individuals’ surgeries took longer to complete than those of the other 2 groups. Long operations in delayed cases were caused, in part, by soft tissue contractures and configuration uncertainty. Additionally, some of these patients sought out traditional care, and improperly administered care had an impact on the conventional surgical approach. Another study discovered that delayed patients resulted in longer surgical times [25]. Closed reduction and percutaneous fixation can be possible in early presenting cases. It has been reported in a study that these patients have a shorter surgical duration than those undergoing open reduction and do not have unaesthetic scarring [26].
Patients in the delayed group had longer incisions than those in the early and elective groups. On the other hand, there was no discernible distinction between the early and elective groups. Wang et al compared patients who underwent surgery within the first 24 h with those who underwent surgery between 24 and 72 h. The authors said that individuals who underwent surgery afterward had longer incisions [25]. In patients who arrive late, swelling and contractures make reduction challenging. Excision of callus tissues is also required. These factors make it possible that the incision can occasionally need to be lengthened.
In our clinic, 2 K-wire applications – the standard procedure for fixing lateral condyle fractures – are used. Due to the significant draw of the extensor muscle groups toward the fragment, a third K-wire can be necessary in some unstable fractures or delayed fractures. Additionally, screws can be chosen over K-wires for early physiotherapy and compression effect when joint motions are constrained in late patients. But when the quantity of K-wires rises, the risk of pin infection rises [20]. The fact that a second surgery is necessary to remove the screws is a drawback. Patients in the delayed group were found to require much more implant use than those in the early group.
Patients who underwent surgery 3 weeks following the injury were examined by Shrestha et al. According to the MEPS, the authors claimed that 70% of patients had excellent results, 28% had good results, and 3% had fair results [14]. In the delayed patient group receiving various treatments, Trisolino et al found that the MEPS rose from 62 before surgery to 98 following surgery [27]. The evaluations for 67% of our patients were excellent, 13% were good, and 20% were fair. Finding varied values in the literature could be the result of surgical variables and study timing differences. Additionally, the surgical outcome may have been impacted by the delayed group applying primarily during the epidemic time.
A negative correlation between time since injury and functional clinical ratings, such as the MEPS, was discovered in a few investigations on delayed groups [10,14]. We also discovered that a considerable delay between the damage and the treatment had a detrimental effect on the treatment results. Additionally, we found that as recovery time from surgery grew, so did the length of the procedure.
Our study has several limitations. First and foremost, its retrospective nature entails inherent limitations. This design carries the risk of selection bias, potentially affecting the study’s conclusions. Additionally, being a single-center study reduces the generalizability of the findings to a broader population. Detailed exploration of socioeconomic factors influencing patients’ delayed presentation and postoperative follow-up was not conducted, leaving these variables insufficiently examined. Metabolic characteristics that could impact fracture healing were not thoroughly detailed. Methodologically, the study exclusively focused on surgically treated patients, missing the opportunity for comparison with a conservative treatment group, which could have provided valuable insights. Furthermore, the use of a 12-h threshold to separate groups might have influenced the group distribution and, consequently, the study outcomes. Additionally, the unequal distribution of patients across groups could have affected the statistical analysis.
Conclusions
The timing of the intervention affects surgical management and clinical outcomes of lateral condyle fractures. Treatments like bringing patients to bonesetters result in delays and additional difficulties in underdeveloped nations. However, in severe global crises, like pandemics, families can become confused and access to medical care can be hampered for a variety of reasons, both internal and external. Despite these, the surgical option is prioritized in the treatment of patients hospitalized for a period of between 3 and 12 weeks. It should be kept in mind that during surgery, the incision can get larger and the procedure can last longer.
Figures
 Figure 1. (A–D) An 8-year-old male patient presenting with a lateral condyle fracture after a playground injury underwent closed reduction and percutaneous pinning. Figure 1 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.
Figure 1. (A–D) An 8-year-old male patient presenting with a lateral condyle fracture after a playground injury underwent closed reduction and percutaneous pinning. Figure 1 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed. 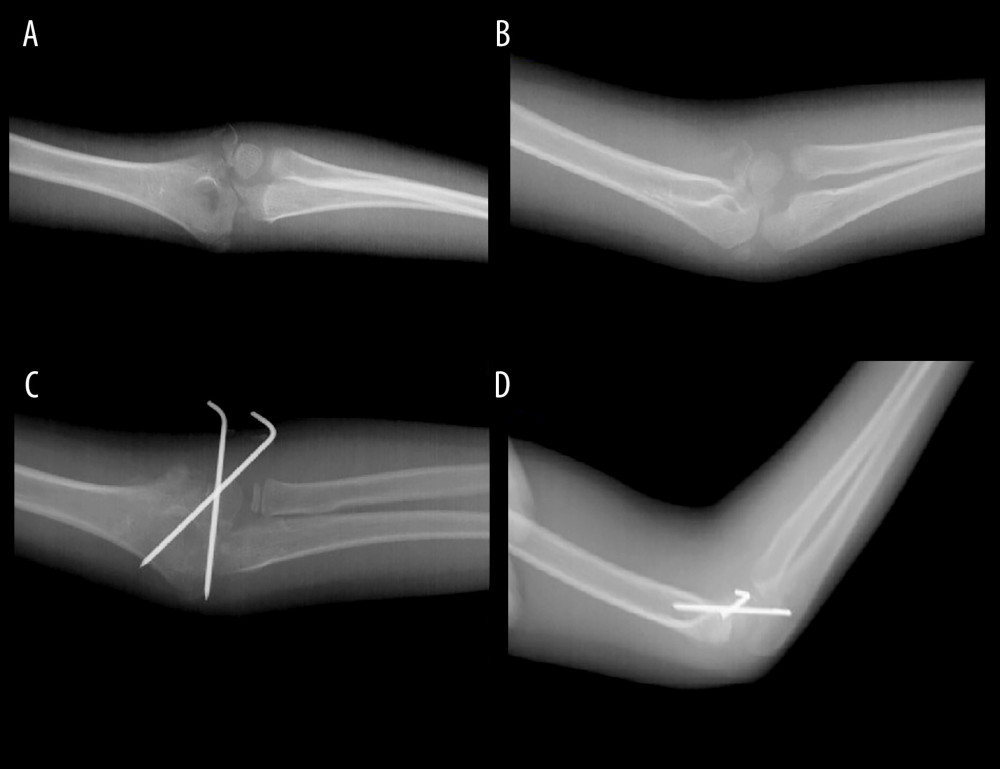 Figure 2. (A–D) The patient with a lateral condyle fracture following a simple fall presented to our facility 3 weeks after the injury. Open reduction and fixation with Kirschner wires were performed for the displaced fracture. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.
Figure 2. (A–D) The patient with a lateral condyle fracture following a simple fall presented to our facility 3 weeks after the injury. Open reduction and fixation with Kirschner wires were performed for the displaced fracture. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed. 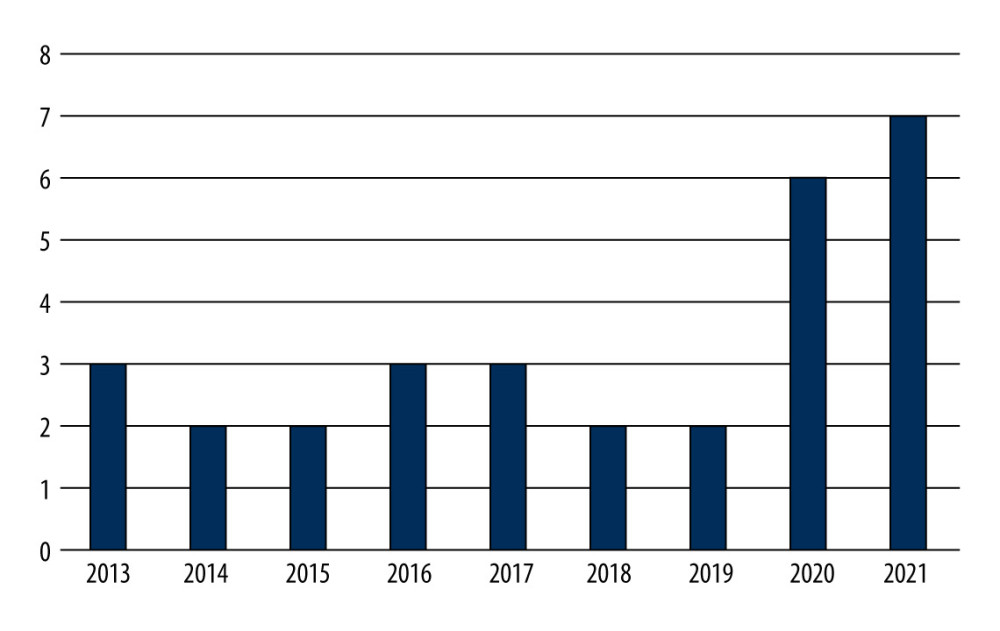 Figure 3. The distribution of patients in the delayed group between 2013 and 2021 shows that patients predominantly sought treatment during the years 2020–2021. Microsoft Excel 2019 software was used to create Figure 3.
Figure 3. The distribution of patients in the delayed group between 2013 and 2021 shows that patients predominantly sought treatment during the years 2020–2021. Microsoft Excel 2019 software was used to create Figure 3. References
1. Abzug JM, Dua K, Kozin SH, Herman MJ, Current concepts in the treatment of lateral condyle fractures in children: J Am Acad Orthop Surg, 2020; 28(1); e9-19
2. Milch H, Fractures and fracture dislocations of the humeral condyles: J Trauma, 1964; 4; 592-607
3. Pirker ME, Weinberg AM, Höllwarth ME, Haberlik A, Subsequent displacement of initially nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: J Trauma, 2005; 58(6); 1202-7
4. Song KS, Kang CH, Min BW, Closed reduction and internal fixation of displaced unstable lateral condylar fractures of the humerus in children: J Bone Joint Surg Am, 2008; 90(12); 2673-81
5. Wu X, Li X, Yang S, Determining the stability of minimally displaced lateral humeral condyle fractures in children: Ultrasound is better than arthrography: J Orthop Surg, 2021; 16(1); 32
6. Haillotte G, Bachy M, Delpont M, The use of magnetic resonance imaging in management of minimally displaced or nondisplaced lateral humeral condyle fractures in children: Pediatr Emerg Care, 2017; 33(1); 21-25
7. James V, Chng ACC, Ting FLM, Lateral condyle fracture of the humerus among children attending a Pediatric Emergency Department: A 10-year single-center experience: Pediatr Emerg Care, 2021; 37(12); e1339-44
8. Cho YJ, Kang SH, Kang MH, K-wire versus screws in the fixation of lateral condyle fracture of humerus in pediatrics: A systematic review and meta-analysis: BMC Musculoskelet Disord, 2023; 24(1); 649
9. Qiao F, Guan X, Jiang F, Lv P, Closed reduction and percutaneous pinning for treatment of unstable lateral condyle fractures of the humerus in children: Front Pediatr, 2023; 11; 1223615
10. Saraf SK, Khare GN, Late presentation of fractures of the lateral condyle of the humerus in children: Indian J Orthop, 2011; 45(1); 39-44
11. Agarwal A, Qureshi NA, Gupta N, Management of neglected lateral condyle fractures of humerus in children: A retrospective study: Indian J Orthop, 2012; 46(6); 698-704
12. Roy MK, Alam MT, Rahman MW, Comparative study of stabilization of humerus supracondylar fracture in children by percutaneous pinning from lateral side and both sides: Mymensingh Med J, 2019; 28(1); 15-22
13. Jakob R, Fowles JV, Rang M, Kassab MT, Observations concerning fractures of the lateral humeral condyle in children: J Bone Joint Surg Br, 1975; 57(4); 430-36
14. Shrestha S, Hutchison RL, Outcomes for late presenting lateral condyle fractures of the humerus in children: A case series: J Clin Orthop Trauma, 2020; 11(2); 251-58
15. Shabir A, Tahir A, Sharief A, Imtiyaz H, Delayed operative management of fractures of the lateral condyle of the humerus in children: Malays Orthop J, 2015; 9(1); 18-22
16. Halvachizadeh S, Teuber H, Cinelli P, Does the time of day in orthopedic trauma surgery affect mortality and complication rates?: Patient Saf Surg, 2019; 13; 8
17. Ozdemir M, Yaradilmis YU, Targal AS, The impact of the COVID-19 pandemic on the orthopaedics outpatient clinic: Eur Rev Med Pharmacol Sci, 2023; 27(1); 431-36
18. Gathen M, Ploeger MM, Peez C, Comparison of the subjective elbow value with the DASH, MEPS und Morrey Score after olecranon fractures: Z Orthopadie Unfallchirurgie, 2020; 158(2); 208-13
19. Mulpruek P, Angsanuntsukh C, Woratanarat P, Shaft-Condylar Angle for surgical correction in neglected and displaced lateral humeral condyle fracture in children: Acta Orthop Belg, 2015; 81(3); 384-91
20. Saris TFF, Eygendaal D, The B, Lateral humeral condyle fractures in pediatric patients: Children (Basel), 2023; 10(6); 1033
21. Muhammad H, Magetsari R, Rukmoyo T, Impacts of COVID-19 pandemic on pediatric fractures: A 4-year evaluation of epidemiology and delayed treatment from prepandemic to pandemic period at a tertiary referral hospital: Ann Med Surg, 2023; 85(9); 4300
22. Rivera-Saldívar G, Martínez-González CA, Manejo y presentación de las fracturas transtrocantéricas de cadera durante la pandemia de COVID-19 en un hospital de tercer nivel de atención: Cir Cir, 2023; 91(3); 368-74 [in Spanish]
23. Huguet Torres A, Carrero Planells AL, Impacto personal y académico de la pandemia por COVID-19 en los estudiantes de enfermería en España (EsE-COVID): Acad J Health Sci Med Balear, 2023; 38(5); 108-16 [in Spanish]
24. Akar MS, Ulus SA, Durgut F, Dönmez S, Complications and difficulties due to bonesetter in the treatment of pediatric distal humerus fractures: J Clin Trials Exp Investig, 2023; 2(1); 38-44
25. Wang B, Gao R, Li Z, Early versus delayed treatment of lateral condylar fracture of the humerus with > 2 mm displacement in children: A retrospective study: J Orthop Surg, 2023; 18(1); 139
26. Xie LW, Deng ZQ, Zhao RH, Closed reduction and percutaneous pinning vs open reduction and internal fixation in pediatric lateral condylar humerus fractures displaced by > 4 mm: An observational cross-sectional study: BMC Musculoskelet Disord, 2021; 22(1); 985
27. Trisolino G, Antonioli D, Gallone G, Neglected fractures of the lateral humeral condyle in children; Which treatment for which condition?: Children (Basel), 2021; 8(1); 56
Figures
 Figure 1. (A–D) An 8-year-old male patient presenting with a lateral condyle fracture after a playground injury underwent closed reduction and percutaneous pinning. Figure 1 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.
Figure 1. (A–D) An 8-year-old male patient presenting with a lateral condyle fracture after a playground injury underwent closed reduction and percutaneous pinning. Figure 1 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.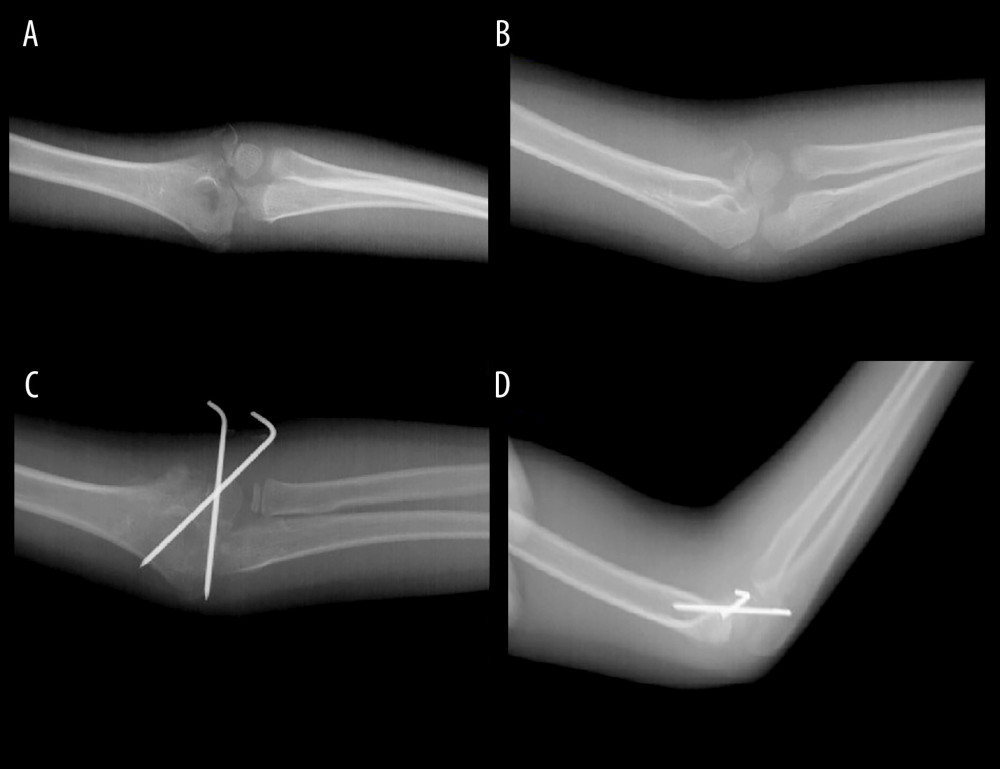 Figure 2. (A–D) The patient with a lateral condyle fracture following a simple fall presented to our facility 3 weeks after the injury. Open reduction and fixation with Kirschner wires were performed for the displaced fracture. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.
Figure 2. (A–D) The patient with a lateral condyle fracture following a simple fall presented to our facility 3 weeks after the injury. Open reduction and fixation with Kirschner wires were performed for the displaced fracture. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.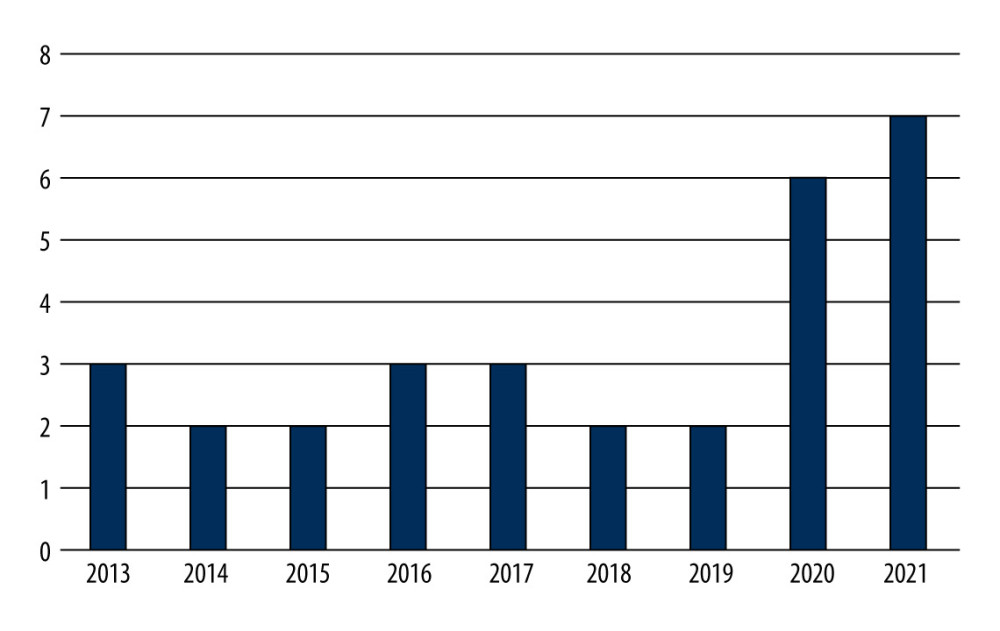 Figure 3. The distribution of patients in the delayed group between 2013 and 2021 shows that patients predominantly sought treatment during the years 2020–2021. Microsoft Excel 2019 software was used to create Figure 3.
Figure 3. The distribution of patients in the delayed group between 2013 and 2021 shows that patients predominantly sought treatment during the years 2020–2021. Microsoft Excel 2019 software was used to create Figure 3. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952